If you have vision-related questions like these, you’re in the right place. We’ve collected educational material here as a one-stop reference for our patients.

One of the most popular ways to correct vision is with a procedure called LASIK (laser in-situ keratomileusis), which uses a laser to change the curvature of the cornea (outer window of the eye). LASIK has quickly become the procedure of choice for most patients because they recover quickly and have fewer side effects and complications than with other methods of vision correction. In fact, most LASIK patients notice a significant improvement in their vision soon after surgery. LASIK removes tissue within the cornea to treat low to high levels of nearsightedness, farsightedness, and astigmatism.
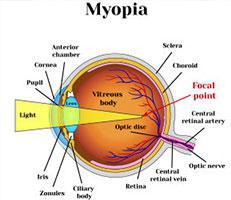
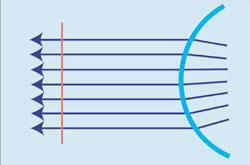
To treat nearsightedness, the steep cornea is made flatter by removing tissue from the center of the cornea. This moves the point of focus from in front of the retina to directly on the retina.
Treating nearsightedness,
the cornea is made flatter
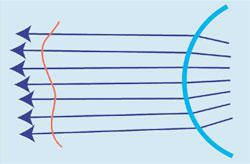
To treat farsightedness, the flat cornea is made steeper by removing tissue outside of the central optical zone of the cornea. This moves the point of focus from behind the retina to directly on the retina.
Treating farsightedness,
the cornea is made steeper
To treat astigmatism, the cornea is made more spherical — like a basketball instead of a football. This eliminates multiple focusing points within the eye and creates one point of focus on the retina. Astigmatism can be treated at the same time as nearsightedness and farsightedness.
Treating astigmatism,
the cornea is made more spherical
LASIK is for those who:
After a thorough eye exam, you and your eye doctor will determine if LASIK is an option for you. If you are a good candidate, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
Since the early 1970’s cataract surgeons have pursued better cataract outcomes by incorporating ultrasonic technology (phacoemulsification) to break up and remove cataracts. Although cataract surgery is considered to be one of the safest and most successful procedures performed in medicine today, laser cataract surgery improves the precision of many key surgical steps to provide even better outcomes and potentially make cataract surgery even safer.
Why Laser Cataract Surgery?
Cataract surgery is one of the safest and most successful procedures in medicine today. Phacoemulsification is still considered the state-of-the-art cataract removal technique, however, there are many steps in the cataract procedure that are still performed manually with microinstruments. Surgeons using the femtosecond laser now perform these steps, adding a greater amount of precision and improved visual outcome to the entire cataract procedure.
The Procedure:
Bladeless Cataract Surgery only takes 10-15 minutes. In addition to using the femtosecond laser to do a number of the surgical steps traditionally performed by hand, we use many of the best innovations in cataract surgery, such as drops only anesthesia (no shots), sutureless incisions through the clear cornea and foldable intraocular lenses. These advances allow us to use the smallest possible incision, approximately 1/18th of an inch.
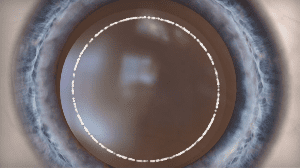
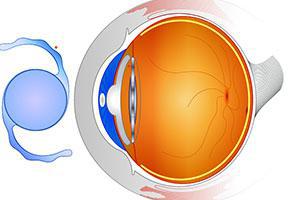
In addition to using the laser to create a stair-stepped, self-sealing incision to begin the procedure, an opening in the thin membrane (capsular bag) that surrounds the natural lens can now be made with the laser. This step, the capsulorhexis, is one of the most delicate steps in cataract surgery and is critical to the efficacy of the procedure. In fact, your replacement Intraocular Lens (IOL) is placed through the capsulorhexis into the capsular bag and it is critical to a good refractive outcome.
The capsulorhexis also provides your surgeon with an opening to begin the removal of the cataract. Once the cataract is removed, the remaining capsular bag serves as a platform to hold the IOL. The round capsulorhexis is usually about 5 millimeters in diameter. If the capsulorhexis not made uniformly it may cause the IOL to tilt or move as the capsular bag contracts around the IOL during the healing process. If the capsulorhexis tears outward during the manual process, it could prevent the insertion of certain types of IOLs.
In traditional cataract surgery, once the capsulorhexis is made manually, the lens has to be chopped into manageable pieces with the ultrasonic power of the phacoemulsification instrument. Certain complications could be induced during this step such as rupturing the posterior surface of the capsular bag and causing injury to the delicate zonular fibers that hold the capsular bag in place and help the natural lens change its shape. In order for the advanced technology toric, multifocal, and accommodating IOLs to function at peak performance, the integrity of the zonular fibers must not be compromised. In order to prevent injury to the zonular fibers, the femtosecond laser is used to gently break apart and soften the cataractous lens.
What are refractive errors?
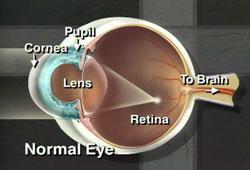
The eye functions similar to a camera with two lenses: the crystalline lens inside the eye and the cornea. The cornea, which is the clear tissue or window covering the front of the eye, is the stronger of the two lenses of the eye and contributes about 2/3 of the focusing power of the eye. For images to be seen clearly, they must be focused on the retina, the light-sensing tissue inside the eye that functions like the film in the camera. An eye that does not require corrective lenses to achieve this is called “emmetropic”. A refractive error—which includes myopia (nearsightedness), hyperopia (farsightedness), and astigmatism—exists if glasses or contact lenses are needed to properly focus images on the retina.
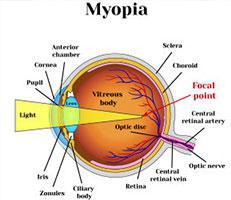
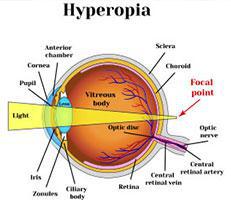
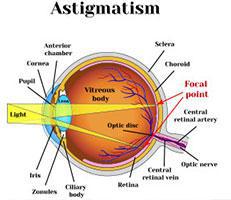
Myopia exists when the focusing power of the eye is too strong and images are focused in front of the retina. This is due to an eye that is too long or a cornea that is too steep. Hyperopia occurs when the focusing power of the eye is too weak and images are focused behind the retina. This condition is caused by an eye that is too short or a cornea that is too flat. Astigmatism is present when the focusing power of the eye is different in different directions so that images are brought to focus at more than one point. This results from uneven corneal curvatures so that the shape of the cornea is more elliptical than spherical (more like a football than a baseball).
Glasses, contact lenses, and refractive surgery are methods of correcting refractive errors.
What is laser vision correction?
Refractive surgery includes many procedures that change the way the eye focuses light on the retina. Laser vision correction is a remarkable advance in refractive surgery for myopia, hyperopia, and astigmatism. The two most common forms of laser vision correction— LASIK (laser in-situ keratomileusis) and PRK (photorefractive keratectomy)—use an FDA approved excimer laser to reshape the cornea to help improve the natural focus of the eye. Excimer laser technology is extremely precise with each pulse of the laser removing microscopic amounts of tissue (0.25 micron) under computerized control. The unpredictability in laser vision correction occurs because every person and every eye heals differently.
The goal of refractive surgery is to reduce one’s need for corrective lenses.
Will I need reading glasses?
If you are over the age of 40, you will probably notice poorer near vision. This is due to the natural aging process of the lens inside the eye and is called presbyopia. Presbyopia cannot be corrected with laser vision correction and therefore you will eventually require reading glasses for near vision. Monovision is an alternative in which one eye is corrected for distance and one eye for near. If you are interested in this option, a monovision trial with contact lenses can be performed prior to surgery to see if you are a good candidate.
What other types of refractive surgery exist?
There are many different procedures that can be used to correct refractive errors. Laser vision correction is currently the most popular type of refractive surgery, but alternatives do exist.
RK (radial keratotomy), which uses deep incisions in the cornea to correct myopia, was very popular prior to laser vision correction but is less predictable and structurally weakens the cornea.
AK (astigmatic keratotomy) is a similar technique in which peripheral corneal incisions are used to reduce astigmatism. This procedure is still utilized, often in conjunction with other techniques.
Intacs are small plastic ring segments that are placed into the peripheral cornea to correct low levels of myopia. Intacs spare the visual axis and are reversible, but the long-term effects of an intracorneal foreign body are not known, and this technique cannot correct moderate or high levels of myopia. Intacs are also being investigated for the correction of hyperopia and astigmatism.
Phakic IOL is a lens implant that is inserted into the eye between the iris (colored portion of the ey) and the natural lens to correct nearsightedness and astigmatism. This procedure is often used for individuals who are not candidates for laser vision correction.
Refractive lens exchange (RLE or presbyopic lens exchange (PRELEX)) is an intraocular surgery in which the natural lens in the eye is removed and replaced with a lens implant. Essentially this is cataract surgery prior to the formation of a cataract. This technique is extremely predictable, however, there are added risks because it is an intraocular procedure rather than just surgery on the surface of the eye.
Thermal keratoplasty (laser (LTK) or conductive energy (CK)) is a technique of heating the peripheral cornea to change its shape and correct low levels of hyperopia. It is extremely safe but the effect tends to fade with time. This procedure has been advertised for correcting presbyopia, however, it does not truly reverse this condition but rather can be used to make the eye slightly nearsighted. This compensates for presbyopia by allowing near vision without glasses, but the distance vision will become blurrier.
Who is a candidate for laser vision correction?
You may be a candidate for LASIK or PRK if you are at least 21 years of age, have healthy eyes, are free of any medical or ocular disorders that may interfere with healing, and have had a stable prescription for a minimum of one year. The amount of correction that has been approved for treatment varies slightly among the different lasers but in general, the lasers are used to treat: nearsightedness between -1.0 and -10.0 D, astigmatism between 0.75 and 4.0 D, and farsightedness between +1.0 and +4.0 D.
While the majority of patients are pleased with their results, no one can promise that you will be able to “throw away your glasses” after surgery. If your goal is to reduce your dependency on glasses or contact lenses, then laser vision correction may be right for you. Understanding the limitations of refractive surgery and having realistic expectations is an important factor for a successful outcome.
Your suitability for the procedure can be determined following a comprehensive eye examination. At that time, special measurements of the eyes will be performed to detect any unseen abnormalities, and you will have the opportunity to have all of your questions answered. If you wear contact lenses, you should discontinue them for at least 1week (soft contacts) or 4 weeks (gas permeable or hard lenses) before this examination, since contact lenses can temporarily change the amount of myopia, hyperopia, and/or astigmatism in your eye and interfere with obtaining accurate measurements.
The decision regarding refractive surgery is a very individual one and you should be fully informed about your options before making a choice. Our goal is to provide the safest and most effective procedure tailored to your individual needs.
What is a wavefront or custom treatment?
All of the laser manufacturers are developing a new generation of laser software to allow for wavefront or customized treatments. The technology is based on individualizing treatments to match the unique refractive errors and aberrations in your eye. A new device is used to measure and map the eye’s optics. This information produces a unique wavefront map or wavescan for each eye, and the wavescan is then used to guide the laser ablation so that a customized treatment is performed. Wavefront treatments may result in improved quality of vision.
What happens during the procedure?
Eye drops are used to anesthetize the eye, a small device called a speculum is positioned to keep your eyelids open and prevent blinking, and you will be asked to look at a fixation light in the laser. The laser portion of the treatment lasts less than 60 seconds and the entire procedure usually takes about 10 minutes.
With LASIK, a thin corneal cap is created with a specialized scalpel called a microkeratome which glides across the surface of the cornea. A suction ring is placed on the eye to stabilize it during this part of the procedure, and while the suction ring is in place, the vision in your eye will gradually dim and then go dark. This is normal and indicates that the appropriate level of suction, to safely make the corneal flap, has been achieved. The suction ring is removed, the flap is folded back, and then the laser treatment is performed on the underlying cornea to reshape the surface. The laser makes a loud clicking/popping noise. The flap is repositioned and held in place by the natural pump mechanism of the cornea.
With PRK, rather than making a flap, the surface cells of the central cornea are gently removed and the laser is applied to the underlying corneal tissue. Then a thin contact lens is placed in the eye as a bandage to help with healing and discomfort.
Two other procedures that are variations of the above, epi-LASIK and LASEK (laser-assisted subepithelial keratectomy), combine the techniques of LASIK and PRK to create a flap of only surface cells without cutting the cornea. Theoretically designed to offer the advantages of both procedures without the complications, epi-LASIK and LASEK have not proven to be any different than PRK except that they take longer to perform.
What are the risks?
All surgical procedures have potential risks. Laser vision correction is a comparatively safe procedure, but complications do occur. Therefore, you should fully understand all the potential risks before undertaking any procedure.
Fortunately, complications are rare and serious complications are very rare. Once the eye heals, you may be under- or overcorrected. In almost all cases, this can be improved by a second procedure. Glare or halos around lights at night are often noticeable (as they can be with contact lenses) but rarely disabling. This phenomenon tends to resolve after 6-12 months but may be permanent. The eyes do get drier after surgery, but this is usually a temporary and asymptomatic effect that improves over 6-12 months. In very rare cases, someone without preexisting dry eye can develop permanent dryness.
There is a very small risk of infection, scarring, or irregular astigmatism, and sometimes these complications may cause a decrease in “best-corrected visual acuity”, which means that your vision with corrective lenses may not be as clear as it was before the surgery. Other complications include healing problems, progressive corneal thinning, or other unexpected results. Any of these, if significant, may require the use of corrective lenses for good vision. In rare instances, as with any eye surgery, vision can be permanently reduced as a result of a complication. In extremely unusual circumstances, additional surgery such as a corneal transplant is needed.
With LASIK, there can also be complications with the corneal flap. If the flap is not perfect, the laser portion of the procedure is not performed. The cornea is allowed to heal and then the surgery can be attempted again. Similarly, adequate suction to create the flap sometimes cannot be achieved and the procedure will have to be rescheduled. Other flap problems include dislocation of the flap, wrinkles in the flap, inflammation under the flap, and surface cells growing underneath the flap. With PRK, steroid drops are used after the surgery for 1 to 4 months, and this carries a small risk of causing high pressure in the eye which may lead to glaucoma. Very rarely a cataract may develop.
The occurrence of a significant complication with laser vision correction is very rare, generally 1% or less. However, even though the risks are low, there is no such thing as risk-free, guaranteed surgery for any condition.
Will I have any pain?
During the surgery, your eye will be anesthetized and you will not feel any pain. With LASIK, some patients notice a pressure sensation from the suction device when the flap is being prepared. After the procedure, there is a variable amount of discomfort. This is more with PRK but is helped with the bandage contact lens and diminishes after several days. If necessary, pain medication may be prescribed.
Which procedure is better?
This is a decision that is best made by you and your doctor. In general, both procedures give similar results for low to moderate levels of correction, while for very high levels of correction, LASIK appears to be more predictable and stable because there is less likelihood of scarring and regression. LASIK also offers the advantages of rapid recovery, less discomfort, and fewer postoperative visits as compared to PRK. However, LASIK requires an additional step (the creation of a flap) and rarely the flap is not perfect and the laser treatment must be delayed.
Whichever procedure you choose, the most important aspect is that you are confident and comfortable with your decision.
What can I expect after surgery?
Patients notice an improvement in vision immediately after laser vision correction. Your vision is initially blurry but clears rapidly over the ensuing days. Some fluctuation in vision may occur for weeks after the treatment. Depending on the type and degree of your refractive error, the chances of seeing 20/40 or better after surgery may exceed 95%.
After LASIK, most people are able to drive and resume work the next day. The healing process is longer with PRK, so patients may not feel comfortable driving or returning to work for several days. The majority of patients undergoing laser vision correction will experience some degree of glare or halos, particularly at night. This improves with time and commonly is not noticed after six months. Some people notice more dryness of the eyes for weeks to months after the surgery. After LASIK, there may be small red patches on the whites of the eye from the suction ring.
Undercorrections or overcorrections may occur, and therefore glasses or contact lenses may be necessary to provide sharper vision. Once the eye has stabilized, usually three months after the initial surgery, a second treatment or enhancement procedure is sometimes performed to fine tune the results.
What restrictions will there be after surgery?
Almost all routine activities may be resumed within 1 to 3 days. You cannot rub your eye for 1 month and should not get water in the eye for 2 weeks. No eye make-up should be worn for 1 week.
 Surgeon experience combined with the latest advances in vision correction technology are the two most important elements that determine how you will see after laser vision correction.
Surgeon experience combined with the latest advances in vision correction technology are the two most important elements that determine how you will see after laser vision correction.
At Mid-Peninsula Ophthalmology Medical Group, we invest heavily training and in leading edge technology. Our commitment to you is that we will not take shortcuts to save you a few dollars. If you are shopping around for vision correction procedures, use this section of our website to compare our technology to others.
 Diagnostic Technology:
Diagnostic Technology:
State-of-the-art diagnostic equipment is important because it’s used to determine whether you are a candidate for laser vision correction, and if so, which procedure is most appropriate for you. It’s also used to calculate the customized settings for the laser for your particular treatment.
Lasers:
Now in its second decade of use, the technologically advanced Excimer laser has added a tremendous amount of precision, control, and safety to treating nearsightedness, farsightedness, and astigmatism. We have a number of Excimer lasers so we can choose the laser that is best suited to treat your specific eye condition.
“It was great! Fast, painless, and easy. For the first time in more than 40 years, I’m able to see without glasses or contacts.”
-Roberta, LASIK patient
“When I first saw you, I was impressed by the detail in which you described the benefits of the procedure, as well as their risks. I quickly felt comfortable in your presence and assured that you would take good care of me. I was surprised to realize how easy the surgery was. The correction in my eyesight is absolutely amazing and has given me a newfound freedom that I appreciate with each passing day. I highly recommend your talent, skill, accessibility and level of care to any patient inquiring about surgery.”
-Stephanie, LASIK patient
“Surgery on the right eye was done elsewhere and required two attempts. I subsequently came to your office on the advice of another physician who is one of your patients and noted how thorough and careful your office was and how he never felt hurried. His description of the office’s practice is exactly what I’ve experienced. I was impressed with the thoroughness with which you evaluated what needed to be done and the time you took to explain as much as I wanted to know. The procedure went as planned and the follow up was excellent. It was a pleasure working with you, and I hope you’ll be available a long time to assist us all with vision care.”
-Stephanie, PRK patient
“The entire experience was marvelous and the results have dramatically changed my life and enjoyment of sports and other activities which were restricted with glasses.”
-William, LASIK patient
“My experience with the surgery and Dr. Friedman were outstanding. It was truly a life-altering experience. I couldn’t be happier.”
-Kevin, LASIK patient
“Thank you for the time you spent with me yesterday. You gave me a lot of good information and didn’t overwhelm me with ophtho-talk. You helped keep me from making a big mistake. I will probably await approval of the phakic IOL. I’m glad people like you are around.”
-Andrea, patient considering LASIK
Laser vision correction is now in its third decade of helping patients reduce or eliminate their dependence on glasses and contact lenses. As testimony to its life-changing benefits, thousands of ophthalmologists and optometrists around the world have become so impressed with the results of laser vision correction that over one million procedures are now performed each year. At Mid-Peninsula Ophthalmology Medical Group our patients continuously tell us they appreciate our commitment to being on the cutting edge of this exciting technology.
Heavy patient demand for laser vision correction has inspired surgeons and laser manufacturers to make tremendous advancements in both Excimer laser technology and surgical technique. When laser vision correction was first performed, only low to moderately nearsighted patients without astigmatism could be treated. Today, with the second and third generation Excimer lasers, very low to moderately high degrees of nearsightedness, farsightedness and astigmatism can be effectively treated. And for many patients that have large pupils, thin corneas or other contraindications for laser vision correction, newer surgical techniques now allow them to enjoy the benefits of clear vision without dependence on glasses and contact lenses.
Laser Vision Correction in Palo Alto at Mid-Peninsula Ophthalmology Medical Group
All laser vision correction procedures are not the same. Because of our dedication to excellence, Mid-Peninsula Ophthalmology Medical Group is recognized as the premium eye care provider in the area. Our surgeons are highly trained in a number of laser vision correction procedures. And we’ve invested in the laser vision technology needed to provide you with the best possible care. Our surgeons have successfully performed thousands of vision correction procedures and are ready to help you choose the option that’s best for your individual vision problem, whether you’re nearsighted, farsighted or have astigmatism.
Pricing
The cost of vision correction varies among practices, based on surgeon experience and what the center includes in the fee. We are not the least expensive providers because we never sacrifice safety to save you money. We have invested heavily in advanced laser technology and our diagnostic technology is second to none. This investment is extremely important to surgical results and our patients tell us they can see the difference.
It’s only natural to want to get the best price, but remember, quality and service are extremely important when it comes to medical care. After all, laser vision correction is a procedure you’ll have only once in your lifetime and your vision is one of your most important assets. The best way to find out exactly what your price will be is to schedule an exam. After a comprehensive evaluation to determine what procedures you’re a candidate for and what degree of correction you need, we’ll be able to give you a specific price.
Insurance companies do not pay for elective vision correction procedures. However, many people have medical flex plans they use to save on their procedure by using pre-tax dollars. Your employer’s human resources department can tell you whether you have this benefit. Vision correction may be tax deductible as a medical expense (check with your financial advisor).
Astigmatic Keratotomy (AK) is an outpatient surgical procedure to reduce or eliminate astigmatism. Astigmatism is caused by a cornea (outer window of the eye) that is shaped like a football, steep in one meridian and flat in the other. In order to reduce or eliminate astigmatism the cornea is reshaped to make it more spherical, like a basketball. AK can be used in combination with RK and other laser and surgical vision correction procedures.
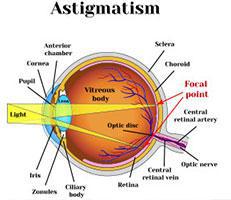
Astigmatism is caused by a cornea (outer
window of the eye) that is shaped like a
football, steep in one meridian and flat in
the other.
AK involves the placement of microscopic incisions in the steeper meridian of the cornea. The incisions cause the cornea to assume a more spherical shape, thereby decreasing the degree of astigmatism.
AK is for those who:
Realistic expectations:
The decision to have AK is an important one that only you can make. The goal of any refractive surgical procedure is to reduce your dependence on corrective lenses. However, we cannot guarantee you will have the results you desire.
After AK, almost everyone experiences some visual side effects. These visual side effects are usually mild and most often diminish over time. But there is a slight chance that some of these side effects won’t go away completely, including light sensitivity, glare, and halos. Serious complications to AK are extremely rare.
If you decide that AK is an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
Alternatives to AK
AK is not the only surgical procedure designed to correct astigmatism. To learn about other procedures, go to the surgical and laser vision correction procedures section of our website.
PRK was the first procedure performed using the Excimer laser. It corrects vision by reshaping the cornea. The difference between LASIK and PRK is that with LASIK a corneal flap is created and the laser is applied to the inner tissue of the cornea. With PRK, the epithelium (or outer skin of the cornea) is removed and a laser is applied to the surface of the cornea. PRK can be used to correct low to high levels of nearsightedness, farsightedness, and astigmatism.

To treat nearsightedness, the steep cornea is made flatter by removing tissue from the center of the cornea. This moves the point of focus from in front of the retina to directly on the retina.
To treat farsightedness, the flat cornea is made steeper by removing tissue outside of the central optical zone of the cornea. This moves the point of focus from behind the retina to directly on the retina.
To treat astigmatism, the cornea is made more spherical — like a basketball instead of a football. This eliminates multiple focusing points within the eye and creates one point of focus on the retina. Astigmatism can be treated at the same time as nearsightedness and farsightedness.
PRK is for those who:
Realistic expectations:
The decision to have PRK is an important one that only you can make. The goal of any refractive surgical procedure is to reduce your dependence on corrective lenses. However, we cannot guarantee you will have the results you desire. The vast majority of our patients are extremely happy with their vision after PRK and can do most activities without dependence on corrective lenses.
PRK is a safe, effective and permanent procedure, but like any surgical procedure, it does have some risks. After PRK, almost everyone experiences some visual side effects.These visual side effects are usually mild and temporary and have a tendency to diminish over time. But there is a slight chance that some of these side effects won’t go away completely, including light sensitivity, glare, and halos. Serious complications to PRK are extremely rare.

PRK is a safe, effective and permanent procedure,
but like any surgical procedure,
it does have some risks.
Since everyone heals somewhat differently, some patients may overreact to the procedure and some may underreact resulting in overcorrections and undercorrections. Once the eye has stabilized (3 to 6 months), you and your doctor can discuss whether a re-treatment could help fine tune your vision if you are over or under corrected.
After a thorough eye exam, you and your doctor will determine if PRK is an option for you. If you are a good candidate, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed.
Alternatives to PRK
PRK is not the only surgical procedure designed to correct nearsightedness, farsightedness, and astigmatism. To learn about other procedures go to the surgical and laser vision correction procedures section of our website.
The word “Phakic” refers to the eye’s natural internal lens. IOL stands for “intra-ocular lens.” In the Phakic IOL procedure, an intraocular lens is placed inside the eye. The patient’s natural lens is not removed, as it would be in cataract surgery. The Implantable Contact Lens, or ICL, is placed between the iris and crystalline lens.
Phakic IOL procedures are being used on severely nearsighted and farsighted patients who may not be candidates for the more common laser procedures such as PRK, LASEK, and LASIK. However, unlike laser vision correction procedures that permanently change your vision, it is possible to remove Phakic IOLs.
Phakic IOLs are for those who:
Realistic expectations:
The decision to have a Phakic IOL is an important one that only you can make. The goal of any vision correction procedure is to reduce your dependence on corrective lenses However, we cannot guarantee you will have the results you desire.
Phakic IOL surgery is considered a relatively new procedure. It is currently being investigated in clinical trials around the world. Serious complications from Phakic IOLs are extremely rare, but like any surgical procedure, it does have some risks.

Serious complications from Phakic IOLs
are extremely rare, but like any surgical
procedure, it does have some risks.
After a thorough eye exam, you and your doctor will determine if phakic IOLs are an option for you. If you are a good candidate, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
Alternatives to Phakic IOLs
Phakic IOLs are not the only surgical procedure designed to correct nearsightedness and farsightedness. To learn about other procedures go to the surgical and laser vision correction procedures section of our website.
RLE is a surgical procedure that uses the same successful techniques of modern cataract surgery. These surgical techniques have evolved and improved dramatically over the last 20 years. Cataract surgery is now the most common surgical procedure performed in medicine today.
The main difference between standard cataract surgery and RLE is that cataract surgery is primarily performed to remove a patient’s cataract that is obstructing and clouding their vision, while RLE is performed to minimize a person’s dependence on glasses or contact lenses.

Cataract surgery is now the most common surgical procedure performed in medicine today.
RLE is for those who:
Cataracts are a part of the normal aging process and if a person lives long enough chances are they will develop cataracts. People who have RLE now will not have cataract surgery in the future.
RLE corrects vision by replacing the eye’s natural lens, which has the wrong focusing power, with an artificial multifocal intra-ocular lens implant that has the correct focusing power for the eye. Having this multifocal lens implant creates a new “visual system” inside the eye, one that can provide the focusing power to see near, intermediate and far images with minimal dependence on corrective lenses. Monofocal lenses, on the other hand, provide clear vision at only one point of focus.
Realistic Expectations

It is extremely important to understand that with multifocal implants you are getting a new “visual system.” You’ve spent years learning how to use your visual system. It will naturally take time for your brain to adjust to a new visual system.
Following RLE, something patients notice right away are halos around objects. On the bottom center is an illustration drawn by a RLE patient representing the appearance of objects immediately after surgery. At the top right, is an illustration representing the appearance of the same objects after the visual cortex of her brain had begun to learn how to process the images. Notice that even the trees and buildings initially have a glow around them but over time the trees and buildings lose their glow and the halos around the car and street lights become less and less noticeable.
The goal of RLE surgery is to reduce or eliminate your dependence on glasses or contact lenses. However, you may not achieve the results you desire and your doctor cannot guarantee your results even if you are considered an ideal candidate.
RLE uses a multifocal lens. This lens has been approved by the FDA for cataract surgery. The FDA has not reviewed this lens for indications other than cataract surgery. Therefore, using a multifocal lens is considered an “off-label” use of an approved medical device if you are younger than 60 and have not been diagnosed with a cataract. Doctors can use approved medical devices when they feel its use is in the best interest of their patients.
Alternatives to RLE
RLE is not the only surgical procedure designed to correct nearsightedness and farsightedness. To learn about other procedures go to the surgical and laser vision correction procedures section of our website.
Radial Keratotomy (RK) is designed to reduce or eliminate myopia, or nearsightedness. Nearsightedness is caused by the cornea being too steep or the eye too long for its corneal curvature. Light rays entering a nearsighted eye focus in front of the retina resulting in blurry vision. RK involves the placement of microscopic incisions outside of the central optical zone. This weakens the outer perimeter of the cornea and causes it to flatten, thereby moving the point of focus from in front of the retina to on the retina.
Radial Keratotomy was very popular in the 80s and early 90s but the advent of the Excimer Laser has added a high degree of accuracy to the correction of nearsightedness with procedures such as PRK and LASIK. RK is still performed on patients who have low to moderate degrees of nearsightedness and simply cannot afford the more expensive laser and surgical correction procedures.
RK is for those who:
Realistic Expectations:
The decision to have RK is an important one that only you can make. The goal of any refractive surgical procedure is to reduce your dependence on corrective lenses. However, we cannot guarantee you will have the results you desire.
After RK, almost everyone experiences some visual side effects. These visual side effects are usually mild and most often diminish over a few days to a few weeks. But there is a slight chance that some of these side effects won’t go away completely, including light sensitivity, glare, and halos. Serious complications to RK are extremely rare. Infection is the most worrisome complication and fortunately, it can usually be eliminated with antibiotic medications.
After a thorough eye exam, you and your doctor will determine if RK is an option for you. If you are a good candidate, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
Alternatives to RK
RK is not the only surgical procedure designed to correct nearsightedness. To learn about other procedures go to the vision correction procedures section of our website.

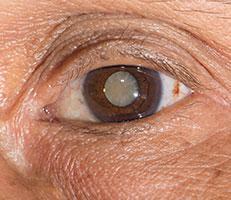
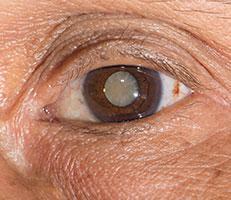
Over fifty percent of people over the age of 60 (and quite a few younger than that) suffer from cataracts. Almost everyone develops cataracts as they grow older. Cataract formations occur at different rates and can affect one or both eyes.
A cataract is a progressive clouding of the eye’s natural lens. It interferes with light passing through the eye to the retina. Aging and other factors cause proteins in the eye’s lens to clump together forming these cloudy areas. Early changes may not disturb vision, but over time cataracts typically result in blurred or fuzzy vision and sensitivity to light. People with progressed cataracts often say they feel as if they’re looking through a waterfall or a piece of wax paper.
Symptoms of Cataracts:
Causes of cataracts:
Diagnosing Cataracts:
Your Menlo Park eye doctor can perform a contrast sensitivity test to determine how much your vision has been affected by a cataract. But typically, when decreased vision affects your everyday activities or hobbies, a cataract should be treated.
Treating Cataracts:
Currently, there is no medical treatment to reverse or prevent the development of cataracts. Once they form, the only way to achieve clear vision again is through cataract surgery.
“Dr. Nakano, I’ve been most pleased with my cataract operations. I want to thank you for your fine efforts to restore my vision. Your skill and attention to detail have opened up a new world.”
—Stan, cataract patient
“Dr. Friedman, I want to thank you for improving my eyesight so tremendously, and without any pain or disability. I can drive again and don’t need eyeglasses!”
—Margaret, cataract patient
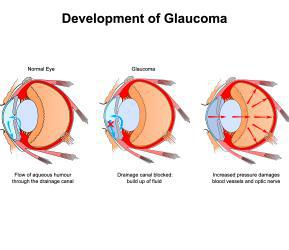
It is estimated that over two million Americans have some type of glaucoma and half of them do not know it. Ninety percent of glaucoma patients have open-angle glaucoma. Although it cannot be cured, it can usually be controlled. Vision loss may be minimized with early treatment. The eye receives its nourishment from a clear fluid that circulates inside the eye.

Fluid circulating inside eye
This fluid must be constantly returned to the blood stream through the eye’s drainage canal, called the trabecular meshwork. In the case of open-angle glaucoma, something has gone wrong with the drainage canal. When the fluid cannot drain fast enough, pressure inside the eye begins to build.
Excess fluid builds pressure
This excess fluid pressure pushes against the delicate optic nerve that connects the eye to the brain. If the pressure remains too high for too long, irreversible vision loss can occur.
Symptoms of Open-Angle Glaucoma:
Who is At Risk
Glaucoma can occur in people of all races at any age. However, the likelihood of developing glaucoma increases if you:
Diagnosing Open-Angle Glaucoma:
Everyone should be checked for glaucoma at around age 35 and again at age 40. Those considered to be at higher risk, including those over the age of 60 should have their pressure checked every year or two.
Your doctor will use tonometry to check your eye pressure. After applying numbing drops, the tonometer is gently pressed against the eye and its resistance is measured and recorded.
An ophthalmoscope can be used to examine the shape and color of your optic nerve. The ophthalmoscope magnifies and lights up the inside of the eye. If the optic nerve appears to be cupped or is not a healthy pink color, additional tests will be run.
Perimetry is a test that maps the field of vision. Looking straight ahead into a white, bowl-shaped area, you’ll indicate when you’re able to detect lights as they are brought into your field of vision. This map allows your doctor to see any pattern of visual changes caused by the early stages of glaucoma.
Gonioscopy is used to check whether the angle where the iris meets the cornea is open or closed. This helps your doctor determine if they are dealing with open-angle glaucoma or narrow-angle glaucoma.
Treatments for Open-Angle Glaucoma:
To control glaucoma, your doctor will use one of three basic types of treatment: medicines, laser surgery, or filtration surgery. The goal of treatment is to lower the pressure in the eye.
Medicines come in pill and eye drop form. They work by either slowing the production of fluid within the eye or by improving the flow through the drainage meshwork. To be effective, most glaucoma medications must be taken between one to four times every day, without fail. Some of these medications have some undesirable side effects, so your doctor will work with you to find a medication that controls your pressure with the least amount of side effects. Medicines should never be stopped without consulting your doctor, and you should notify all of your other doctors about the medications you are taking.
Argon Laser Trabeculoplasty and Selective Laser Trabeculoplasty surgery treat the drainage canal. Requiring only numbing eye drops, the laser beam is applied to the trabecular meshwork resulting in an improved rate of drainage. When laser surgery is successful, it may reduce the need for daily medications.
Laser Surgery Can Reduce the Need for Daily Medication
Filtration surgery is performed when medicines and/or laser surgery are unsuccessful in controlling eye pressure. During this microscopic procedure, a new drainage channel is created to allow fluid to drain from the eye.
 Narrow-angle glaucoma is much rarer and is very different from open-angle glaucoma in that eye pressure usually goes up very fast. This happens when the drainage canals get blocked or covered over. The iris gets pushed against the lens of the eye, shutting off the drainage angle. Sometimes the lens and the iris stick to each other. This results in pressure increasing suddenly, usually in one eye. There may be a feeling of fullness in the eye along with reddening, swelling, and blurred vision.
Narrow-angle glaucoma is much rarer and is very different from open-angle glaucoma in that eye pressure usually goes up very fast. This happens when the drainage canals get blocked or covered over. The iris gets pushed against the lens of the eye, shutting off the drainage angle. Sometimes the lens and the iris stick to each other. This results in pressure increasing suddenly, usually in one eye. There may be a feeling of fullness in the eye along with reddening, swelling, and blurred vision.
Symptoms of Narrow-Angle Glaucoma:
The onset of acute narrow-angle glaucoma is typically rapid, constituting an emergency. If not treated promptly, this glaucoma produces blindness in the affected eye in three to five days. Symptoms may include:
Causes of Narrow-Angle Glaucoma:
Diagnosing Narrow-Angle Glaucoma:
Everyone should be checked for glaucoma at around age 35 and again at age 40. Those considered to be at higher risk for narrow-angle glaucoma, including those who are Asian, farsighted or over the age of 60, should have their pressure checked every year or two.
Because of the rapid, potentially devastating results of narrow-angle glaucoma, you should seek medical treatment immediately if you experience any of the above symptoms.
During eye exams, your doctor will use tonometry to check your eye pressure. After applying numbing drops, the tonometer is gently pressed against the eye and its resistance is measured and recorded.
An ophthalmoscope can be used to examine the shape and color of your optic nerve. The ophthalmoscope magnifies and lights up the inside of the eye. If the optic nerve appears to be cupped or is not a healthy pink color, additional tests will be run.
Gonioscopy is used to determine whether the angle where the iris meets the cornea is open or closed, a key difference between open-angle glaucoma and narrow-angle glaucoma.
Treatment for Narrow-Angle Glaucoma:
Laser iridotomy is a common treatment for narrow-angle glaucoma. During this procedure, a laser is used to create a small hole in the iris, restoring the flow of fluid to the front of the eye. In most patients, the iridotomy is placed in the upper portion of the iris, under the upper eyelid, where it cannot be seen.
Filtration surgery is performed when medicines and/or laser surgery are unsuccessful in controlling eye pressure. During this microscopic procedure, a new drainage channel is created to allow fluid to drain from the eye.

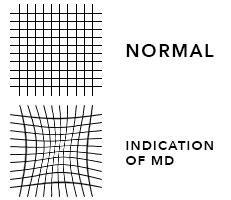
Macular degeneration is a disease of the macula, an area of the retina at the back of the eye that is responsible for fine detail vision. Vision loss usually occurs gradually and typically affects both eyes at different rates. Even with a loss of central vision, however, color vision and peripheral vision may remain clear.
Symptoms of Macular Degeneration:

There are two forms of age-related macular degeneration, wet and dry.
Wet Macular Degeneration
Wet macular degeneration occurs when abnormal or leaking blood vessels grow underneath the retina in the area of the macula. These changes can lead to distorted or blurred vision and, in some cases, a rapid and severe loss of straight ahead vision.
Dry Macular Degeneration
The vast majority of cases of macular degeneration are the dry type, in which there is thinning or deterioration of the tissues of the macula or the formation of abnormal yellow deposits called drusen. Progression of dry macular degeneration occurs very slowly and does not always affect both eyes equally.
Causes of or Contributing Factors to Macular Degeneration:
The root causes of macular degeneration are still unknown. Women are at a slightly higher risk than men. Caucasians are more likely to develop macular degeneration than African Americans.
Diagnosing Macular Degeneration:
Your eye doctor can identify changes of the macula by looking into your eyes with various instruments. A chart known as an Amsler Grid can be used to pick up subtle changes in vision.
Angiography is the most widely used macular degeneration diagnostic test. During the test, a harmless orange-red dye called Fluorescein will be injected into a vein in the arm. The dye travels through the body to the blood vessels in the retina. A special camera takes multiple photographs. The pictures are then analyzed to identify damage to the lining of the retina or atypical new blood vessels. The formation of new blood vessels from blood vessels in and under the macula is often the first physical sign that macular degeneration may develop.
Optical Coherence Tomography (OCT) uses light waves to create a contour map of the retina and can show areas of thickening or fluid accumulation.
Treatment for Macular Degeneration:
In the early stages of macular degeneration, regular eye check-ups, attention to diet, in-home monitoring of vision and possibly nutritional supplements may be all that is recommended.
Diet and Nutritional Supplements
There has been active research on the use of vitamins and nutritional supplements called antioxidants to try to prevent or slow macular degeneration. Antioxidants are thought to protect against the damaging effects of oxygen-charged molecules called free radicals. A potentially important group of antioxidants are called carotenoids. These are the pigments that give fruits and vegetables their color. Two carotenoids that occur naturally in the macula are lutein and zeaxanthin. Some research studies suggest that people who have diets high in lutein and zeaxanthin may have a lower risk of developing macular degeneration. Kale, raw spinach, and collard greens are vegetables with the highest amount of lutein and zeaxanthin. You can also buy nutritional supplements that are high in these and other antioxidants.
Low Vision Aids
Unfortunately, the vast majority of cases of wet macular degeneration and virtually all cases of dry macular degeneration are not treatable. In these cases, low vision aids may help make it easier to live with the decreased vision of macular degeneration. Low vision aids range from hand-held magnifying glasses to sophisticated systems that use video cameras to enlarge a printed page. Lifestyle aids such as large print books, tape-recorded books or magazines, large print playing cards, talking clocks and scales and many other devices are available.
Laser Treatments
In rare cases of wet macular degeneration, laser treatment may be recommended. This involves the use of painless laser light to destroy abnormal, leaking blood vessels under the retina. This form of treatment is only possible when the abnormal blood vessels are far enough away from the macula that it will not damage it. Only rare cases of wet macular degeneration meet these criteria. When laser treatment is possible, it may slow or stop the progression of the disease but is generally not expected to bring back any vision that has already been lost.
A relatively new form of treatment for some cases of wet macular degeneration is called photodynamic therapy or PDT. In those cases where PDT is appropriate, slowing of the loss of vision and sometimes, even improvement in vision are possible.
See “Eye Conditions” below.
 Most likely, your eyes are the first thing people notice about your appearance. They are probably the most important aspect of facial attractiveness. Unfortunately, even with a good night’s sleep, loose skin over your eyes or bags under your eyes can make you look tired or sad, or older than you really are. As we go through life, even if we have taken care of ourselves, the skin around our eyes stretches and wrinkles. Fatty deposits cause the upper lids to sag, while under the eye the tissue bulges forward and becomes discolored. In severe cases, vision can become partially blocked.
Most likely, your eyes are the first thing people notice about your appearance. They are probably the most important aspect of facial attractiveness. Unfortunately, even with a good night’s sleep, loose skin over your eyes or bags under your eyes can make you look tired or sad, or older than you really are. As we go through life, even if we have taken care of ourselves, the skin around our eyes stretches and wrinkles. Fatty deposits cause the upper lids to sag, while under the eye the tissue bulges forward and becomes discolored. In severe cases, vision can become partially blocked.
Causes of Droopy Eyes:

Treatment for baggy eyes: The most common treatment for baggy eyes is called blepharoplasty or eyelid surgery. We offer a number of finance options and affordable payment plans. It is easy to apply online to receive credit approval before you schedule an appointment.
The Menlo Park eye doctors at Mid-Peninsula Ophthalmology Medical Group are totally committed to remaining on the cutting-edge of ophthalmic innovation and technology. We continually invest in state-of-the-art diagnostic and surgical equipment. Our doctors go through rigorous, ongoing training to ensure that we’re doing everything we can to improve our patients’ vision and quality of life. We know our focus on technology is worth the investment and our patients tell us they can truly see the difference.
Our commitment to our patients, evidenced by our investment in technology, is why we have so much information on our Web site. We want our patients to recognize that there is a difference in eye care providers. Eye care and vision correction have come a long way since the days when an individual’s only option was a new pair of glasses. Our Menlo Park eye doctors are now using breakthrough treatments that have improved vision for millions of patients of all ages and from all walks of life.
Ophthalmic surgery is now a precise, sophisticated science, where surgeons rely on advanced technology to diagnose and treat problems such as glaucoma, corneal disease, macular degeneration, diabetic retinopathy, and cataracts. Many procedures that used to require a hospital stay and lengthy recovery are now performed on an outpatient basis with most patients returning to their normal activities the next day.
And thanks to new laser vision correction technology, millions who were nearsighted, farsighted, presbyopic or had astigmatism are now free of glasses and contacts. Heavy patient demand for surgical and laser vision correction has inspired surgeons and laser manufacturers to make tremendous advancements in both Excimer laser technology and surgical technique.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
See “Eye Conditions” below.
We were all born with smooth, baby-soft skin. When we were children, the muscles under our skin contracted to display facial lines of emotion, signifying happiness or sadness. As soon as our emotions returned to normal, our expression lines disappear.
But as we go through a lifetime of emotions and our skin begins to lose its elasticity, those facial lines do not go away completely, making us look older than we feel. Our skin becomes a road map showing the effects of where we have been and what we have done.
Causes of Facial Wrinkles:
Treatment for Facial Wrinkles:
There are several cosmetic procedures that can reduce facial wrinkles.
We offer a number of finance options and affordable payment plans. It is easy to apply online to receive credit approval before you schedule an appointment.
See “Eye Conditions” below.

See “Vision Correction” above.
Over fifty percent of people over the age of 60 and quite a few younger than that suffer from cataracts. Currently, there is no medical treatment to reverse or prevent the development of cataracts. Once they form, the only way to see clearly again is to have them removed from within the eye.
In your parents’ or grandparents’ day, cataract surgery was considered risky, required a lengthy hospital stay, and was usually postponed for as long as possible. Today, cataract surgery is performed on an outpatient basis and takes only a few minutes. It is now one of the most common and successful medical procedures performed. In fact, following cataract surgery, many patients experience vision that is actually better than what they had before they developed cataracts. See what our Palo Alto cataract patients have to say about their cataract surgery.
Cataract surgery is for those who:
What to expect on your cataract surgery day:
You will arrive at the Palo Alto eye surgery center about an hour prior to your procedure. Once you have been checked in you may be offered a sedative to help you relax. You will then be prepared for surgery. The area around your eyes will be cleaned and a sterile drape may be applied around your eye.
Eye drops or a local anesthetic will be used to numb your eyes. When your eye is completely numb, an eyelid holder will be placed between your eyelids to keep you from blinking during the procedure.
A very small incision will be made and a tiny ultrasonic probe will be used to break up the cataract into microscopic particles using high-energy sound waves. This is called phacoemulsification.
The cataract particles will be gently suctioned away. Then, a folded intraocular lens (IOL) will be inserted through the micro-incision, then unfolded and locked into permanent position. The small incision is “self-sealing” and usually requires no stitches. It remains tightly closed by the natural outward pressure within the eye. This type of incision heals fast and provides a much more comfortable recuperation.
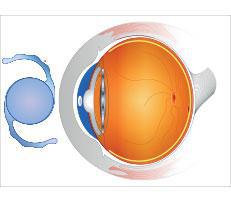
Intra-Ocular Lens replaces the natural lens of the eye. The IOL is placed inside the capsular bag of the eye.
If your eye has pre-existing astigmatism, your surgeon may elect to make micro-incisions in the cornea to reduce your astigmatism. These are called LRIs or limbal relaxing incisions.
You will go home soon after the surgery and relax for the rest of the day. Everyone heals somewhat differently, but many patients report improvement in their vision almost immediately after the procedure. Most patients return to their normal activities within a day or two.
Realistic expectations:
The decision to have cataract surgery is an important one that only you can make. The goal of any vision restoration procedure is to improve your vision. However, we cannot guarantee you will have the results you desire.
Once removed, cataracts will not grow back. But some patients may experience clouding of a thin tissue, called the capsular bag, that holds the intra-ocular lens. In most cases, a laser is used to painlessly open the clouded capsule and restore clear vision with a procedure called a capsulotomy.
The capsular bag may become cloudy in the future.
Serious complications with cataract surgery are extremely rare. It is a safe, effective and permanent procedure, but like any surgical procedure, it does have some risks. Going to an eye specialist experienced with the procedure can significantly minimize the risks involved with cataract surgery.
After a thorough eye exam, you and your Menlo Park eye doctor will determine if cataract surgery is an option for you. You will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
You may also choose to make an appointment or request additional information to learn more about this exciting procedure.
See “Vision Correction” above.
The Menlo Park eye doctors at Mid-Peninsula Ophthalmology Medical Group are totally committed to remaining on the cutting-edge of ophthalmic innovation and technology. We continually invest in state-of-the-art diagnostic and surgical equipment. Our doctors go through rigorous, ongoing training to ensure that we’re doing everything we can to improve our patients’ vision and quality of life. We know our focus on technology is worth the investment and our patients tell us they can truly see the difference.
Our commitment to our patients, evidenced by our investment in technology, is why we have so much information on our website. We want our patients to recognize that there is a difference in eye care providers. Eye care and vision correction have come a long way since the days when an individual’s only option was a new pair of glasses. Our Menlo Park eye doctors are now using breakthrough treatments that have improved vision for millions of patients of all ages and from all walks of life.
Ophthalmic surgery is now a precise, sophisticated science, where surgeons rely on advanced technology to diagnose and treat problems such as glaucoma, corneal disease, macular degeneration, diabetic retinopathy, and cataracts. Many procedures that used to require a hospital stay and lengthy recovery are now performed on an outpatient basis with most patients returning to their normal activities the next day.
And thanks to new laser vision correction technology, millions who were nearsighted, farsighted, presbyopic or had astigmatism are now free of glasses and contacts. Heavy patient demand for surgical and laser vision correction has inspired surgeons and laser manufacturers to make tremendous advancements in both Excimer laser technology and surgical technique.

The only effective treatment for cataracts is surgery. While the word surgery can frighten some people, modern medical technology allows your cataract to be treated safely with a microsurgical technique that takes less than 20 minutes to perform. Each year in the United States, about 3.5 million people have their cataracts removed and an artificial lens put in its place.
Once the cataract is removed, a permanent, artificial lens, called an intraocular lens or IOL is implanted. There are two types of IOLs available; non-foldable and foldable. Non-foldable IOLs are made of a hard plastic material. Alcon Acrysof is a foldable lens made of a soft acrylic material. A dedicated research and development team took 10 years to develop, test and bring this product to market.
For most cataract patients, life without reading glasses or bifocals is something they either experienced before presbyopia or they just dreamed about for most of their lives. But today, The AcrySof® IQ ReSTOR® IOL is turning those dreams into reality with its revolutionary lens technology, which allows patients to see clearly at all distances, day or night, without bifocals or reading glasses. The AcrySof® IQ ReSTOR® IOL is now available and delivers a high level of glasses-free vision.
The AcrySof® IQ ReSTOR® IOL is a second generation multifocal lens that provides excellent near to distant vision and greatly reduces their reliance on reading glasses or bifocals. The AcrySof® IQ ReSTOR® IOL is an artificial lens used in cataract surgery for patients with and without presbyopia.
The AcrySof® IQ ReSTOR® IOL also has an “aspheric” surface that has proven to eliminate much of the night vision distortions and loss of contrast that can be experienced with standard IOLs.
Presbyopia occurs when the natural lens inside the eye loses its ability to change shape and eventually affects everyone, including those who are nearsighted, farsighted, have cataracts, or had perfect vision most of their life.
AcrySof® IQ ReSTOR® provides a full range of vision, decreasing
dependence on reading glasses or bifocals.
Say “goodbye” to both cataracts and astigmatism at the same time. Say “hello” to a clear tomorrow!
Traditionally patients receive a monofocal IOL that generally provides good distance vision without glasses or contacts. However, many patients that also have astigmatism will still experience blurry distance vision because standard IOLs do not correct astigmatism. Corrective eyewear or additional surgery is needed to reduce blurring and distortion caused by astigmatism.
Astigmatism occurs when the cornea is shaped like a football (more curved in one direction than the other) which causes light to focus in more than one point on the retina and thus results in blurry, distorted vision.
Today, patients with astigmatism who want freedom from glasses for distance vision after cataract surgery can choose to have the AcrySof® IQ Toric IOL.
The AcrySof® IQ Toric IOL not only clears vision when the cataract is removed, it can reduce or eliminate the blurring and distortion caused by astigmatism. The AcrySof® IQ Toric IOL has a unique “aspheric” surface that has proved to eliminate much of the night vision distortions and loss of contracts that can be experienced with standard IOLs.
For more information visit www.acrysofiqtoric.com.
Corneal topography is a computer assisted diagnostic tool that creates a three-dimensional map of the surface curvature of the cornea. The cornea (the front window of the eye) is responsible for about 70 percent of the eye’s focusing power. An eye with normal vision has an evenly rounded cornea but if the cornea is too flat, too steep, or unevenly curved, less than perfect vision results. The greatest advantage of corneal topography is its ability to detect irregular conditions invisible to most conventional testing.
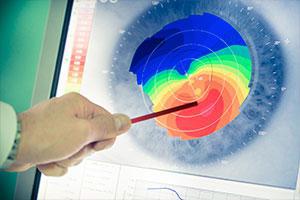
Corneal topography produces a detailed, visual description of the shape and power of the cornea. This type of analysis provides your doctor with very fine details regarding the condition of the corneal surface. These details are used to diagnose, monitor, and treat various eye conditions. They are also used in fitting contact lenses and for planning surgery, including laser vision correction. For laser vision correction the corneal topography map is used in conjunction with other tests to determine exactly how much corneal tissue will be removed to correct vision and with what ablation pattern.
Computerized corneal topography can be beneficial in the evaluation of certain diseases and injuries of the cornea including:
The corneal topography equipment consists of a computer linked to a lighted bowl that contains a pattern of rings. During a diagnostic test, the patient sits in front of the bowl with his or her head pressed against a bar while a series of data points are generated. Computer software digitizes these data points to produce a printout of the corneal shape, using different colors to identify different elevations, much like a topographic map of the earth displays changes in the land surface. The non-contact testing is painless and brief.
Doctors have been routinely treating nearsightedness, farsightedness, and astigmatism with incisional procedures such as Radial Keratotomy and Astigmatic Keratotomy for over 25 years. By the early 1980s, they began looking at lasers to improve the precision and predictability of altering the shape of the cornea. Researchers found that IBM’s new Excimer laser, used initially for etching computer chips, had medical applications as well. Now in its second decade of use, the technologically advanced Excimer laser has added a tremendous amount of precision, control, and safety to treating nearsightedness, farsightedness, and astigmatism.

Its ability to remove corneal tissue with accuracy up to 0.25 microns (0.00004 of an inch) with each pulse makes the Excimer laser so well suited for correcting vision. Often, only 50 microns of tissue (about the thickness of a human hair) are removed to achieve the proper amount of correction.
The Excimer laser produces a “cool” light beam that does not damage surrounding tissue. High-energy photons from the laser break the molecular bonds a few layers a time.
At Mid-Peninsula Ophthalmology Medical Group we have several Excimer lasers so our doctors can match the unique characteristics of your eye to the unique capabilities each of our lasers provide.

Visual field testing is an important tool in the diagnosis and management of glaucoma. It is used to confirm that glaucoma has affected the visual function, to evaluate the severity and to monitor the progression of the disease. The Humphrey Field Analyzer II is a wheelchair accessible diagnostic tool used to examine a patient’s visual field. The Humphrey Field Analyzer II is the recognized standard of care for early diagnosis and management of ocular diseases resulting in visual field loss.
Why we’ve invested in the Humphrey Field Analyzer II

The only treatment for cataracts today is to remove the cataract and replace it with a clear artificial lens known as an intraocular lens (IOL). Cataract surgery is safer, faster, and more comfortable than ever before and millions of people worldwide are now enjoying excellent vision as a result of their cataract procedure
The Tecnis™ IOL is approved by the FDA to improve functional vision, which is likely to provide a meaningful safety benefit for older drivers. Our eyes, like other parts of our body, actually fall out of balance with age. When we’re young, the eye’s two focusing lenses, the cornea (outer lens of the eye) and natural crystalline lens, actually work together to focus light onto the retina. As we age, the natural lens loses some of its ability to balance the cornea, resulting in vision that it is not quite as crisp as it used to be. The Tecnis™ lens is designed to restore this balance to a level more like that of a healthy person in their 20s.

While most IOLs are made with a rounded surface, the Tecnis™ IOL was developed through advanced wavefront modeling of human corneas. The modified lens surface works with the cornea in a way that more closely resembles the balance of a natural lens and cornea of a younger person. The result is improved functional vision after cataract surgery.
While traditional lens implants may improve your vision, only the TECNIS™ lens improves functional vision as was shown clinically in night driving simulator testing. Based on these test results, the TECNIS™ IOL is likely to provide a meaningful safety benefit for older drivers and the drivers and pedestrians with whom they share the road.
Chances are, several of your friends or family members are experiencing the joys of living without glasses and contact lenses as a result of laser vision correction. You’ve heard the excitement in their voices, noticed the boost in their confidence levels, and watched the quality of their lives improve with new-found freedoms. Millions of Americans are enjoying these life-enhancing benefits and millions more, just like you, are exploring the procedure that could free them from the worries of glasses and contact lenses.
VISX CustomVue™ Improves the View of Laser Vision Correction
CustomVue™ Individualized Laser Vision Correction was developed by VISX, the company recognized worldwide for bringing innovation and breakthrough technology to laser vision correction. With CustomVue, a new standard in laser vision correction is established, providing a precise level of measurement and correction never before possible.
Using WaveScan®-based digital technology, originally developed for use in high-powered telescopes to reduce distortions when viewing distant objects in space, doctors can now identify, measure, and correct imperfections in an individual’s eyes 25 times more precisely than with standard methods used for glasses and contact lenses. This information is transferred to the laser, providing a new level of precision and accuracy.
Reach the Full Potential of Your Vision—Your Personal Best Vision
Just like a fingerprint, each person’s vision is 100 percent unique to their eyes. Before the recent advancements in technology, doctors were only able to use standard measurements to correct vision, meaning that prescriptions could only provide a certain level of correction regardless of an individual’s needs.
Now, VISX CustomVue can measure and correct the unique imperfections of each individual’s vision and provide them with the potential to experience better vision than is possible with glasses or contact lenses—Personal Best Vision.
Taking the Mystery out of Laser Vision Correction
The laser vision correction process begins with a consultation with your doctor where a patient can learn about the technology and the procedure.
An evaluation follows to assess a patient’s overall health and to measure and create a detailed and unique map of their eyes. Once it’s confirmed that an individual is a good candidate for laser vision correction, the procedure can be scheduled.
On the day of the procedure, anesthetic drops are placed into the patient’s eyes. The patient’s unique correction information is transferred from the WaveScan to the laser. Laser vision correction works by gently reshaping the cornea with the cool beam from the laser to remove microscopic amounts of tissue—less than the thickness of a human hair in most cases—to create a new curvature. The procedure typically takes several seconds and the majority of individuals feel no discomfort. Many patients notice immediate results after CustomVue and vision continues to improve over several days. Routine follow-up visits complete the process.
VISX® lasers have been used to perform millions of laser vision correction procedures in the U.S. and around the world. If you’re over the age of 21 and are nearsighted and/or astigmatic, you may be a candidate for the CustomVue procedure.
The first step is to call Mid-Peninsula Ophthalmology Medical Group to schedule a consultation. During the consultation, you can review the details of the technology and the procedure and be that much closer to living your best life with your Personal Best Vision. If you have any questions, or for more information about CustomVue, visit www.personalbestvision.com.

VISX laser systems have been used to perform millions of laser vision correction procedures in the U.S. and around the world. Every year, more doctors use VISX lasers to perform laser vision correction surgery than any other system. The VISX STAR S4 is one of the most advanced systems on the market today. This technologically advanced laser offers faster treatments using variable spot beam technology and an eye tracking system that tracks in all three dimensions.
The VISX STAR S4 can be used in combination with VISX CustomVue™ to address the unique imperfections of each individual’s vision. CustomVue can provide our patients with the potential to experience better vision than is possible with glasses or contact lenses.
Why we’ve chosen the VISX STAR S4 Excimer Laser System:
For more information about the VISX STAR S4 Excimer Laser System, go to http://www.visx.com.
No two eyes are the same. Like your DNA or fingerprint, your vision is unique.
Until now, laser vision correction treatment was based on diagnostic technology similar to that used for the prescription eyeglasses or contact lenses. The new WavePrint™ System by VISX takes laser vision correction to an entirely new, personalized level by combining exclusive personalized diagnostic technology and the Excimer laser into one system.
The advanced diagnostic portion of the technology produces a precise, detailed analysis of your vision and provides a personalized laser vision correction plan that addresses your individual needs. This WavePrint Map is coordinated with the VISX STAR S3 ActiveTrak™ Excimer Laser System to create one of the most advanced systems on the market. The eye tracker adds a new level of precision, comfort, and safety.
Why we’ve chosen the VISX Waveprint™ System:
For more information about the VISX Waveprint™ System, go to http://www.visx.com.
Until recently, laser vision correction treated patients based strictly on their optical prescription. In other words, if you were a minus-four nearsighted person, glasses with minus-four lenses would get you back to seeing the best that you could. If you had laser vision correction, that same prescription would be programmed into the excimer laser and the exact amount of tissue would be removed to make a minus-four into a zero. Anyone who was a minus-four would get the exact same treatment. We call this conventional laser vision correction.
Today, with the advent of wavefront diagnostic technology, wavefront-guided excimer lasers can now treat patients according to the uniqueness of their entire optical system, not just their prescription.
How It Works
Wavefront technology was pioneered for astronomy and physics to aid in reducing aberrations or imperfections in the optical systems of telescopes. In much the same way, wavefront-sensing devices are being used to produce an accurate picture of the optical imperfections found in the human eye. This technology differs from traditional testing methods in its ability to measure the entire optical system of the eye, instead of simply the front surface of the eye. Light travels in a procession of flat sheets known as wavefronts. These wavefronts enter the eye, pass through the entire optical system (the cornea, lens, and retina) and are then reflected back. When the optical system has perfect refracting surfaces, these wavefronts exit the eye as flat sheets. But when the cornea is irregular or the lens is imperfect, higher-order aberrations are created, and the wavefronts exit the eye as irregular, curved sheets.
Perfect Eye Returning Wavefront
Aberrated Eye Returning Wavefront
Wavefront technology captures the reflected wavefronts and compares these curved sheets to a perfect wavefront and a 3-D map of the eye’s optical irregularities is created. This map is then transferred to the excimer laser and is used as a guide to reshape the cornea during laser vision treatment.
Results have shown that custom laser vision correction can reduce some of the unwanted visual effects experienced from conventional laser vision correction, especially those associated with night vision such as glare and halos. By addressing both a person’s prescription and the higher order aberrations within their eye’s optical system, custom laser vision correction has the potential of making patients see better than they could with conventional glasses or conventional laser vision correction.

See “Ophthalmology Technology at MPOMG” above.
See “Vision Correction” above.
See “Vision Correction” above.
 Laser surgery has become increasingly popular as an intermediate step between drugs and traditional glaucoma surgery. The most common type of laser surgery performed for open-angle glaucoma is called Argon Laser Trabeculoplasty (ALT). The objective of the surgery is to help fluids drain out of the eye, reducing intra-ocular pressure that can cause damage to the optic nerve and loss of vision.
Laser surgery has become increasingly popular as an intermediate step between drugs and traditional glaucoma surgery. The most common type of laser surgery performed for open-angle glaucoma is called Argon Laser Trabeculoplasty (ALT). The objective of the surgery is to help fluids drain out of the eye, reducing intra-ocular pressure that can cause damage to the optic nerve and loss of vision.
Although your eye care professional may suggest ALT surgery at any time, it is often performed after trying to control intra-ocular pressure with medicines. In many cases, you will need to keep taking glaucoma medications even after ALT surgery.
ALT is for those:
Realistic expectations:
The effect of the surgery may wear off over time. Two years after ALT surgery, the pressure from glaucoma increases again in more than half of all patients. Serious complications with ALT are extremely rare, but like any surgical procedure, it does have some risks. You will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
See “Vision Correction” above.
A comprehensive eye exam will evaluate not only how well you see but also identify potential eye diseases. Some eye diseases, such as glaucoma and macular degeneration, can result in serious vision loss if not detected and treated early. Often, patients with these diseases don´t experience any visual symptoms before vision loss occurs.
If you are over 35, you should have a comprehensive eye exam every two years. Patients over 65 or with a family history of glaucoma, diabetes, or diabetic retinopathy should have a yearly eye exam.
What to expect at your eye exam:
Your doctor will most likely dilate the pupils of your eyes, in order to better see the retina at the back of your eye. You may want to consider making transportation arrangements, as your vision may be blurry for a few hours after dilating.
Your exam may include a:
Treatment options, if necessary will be presented at the conclusion of your examination.
To schedule a comprehensive eye exam, you can call our office or schedule an exam.
Laser iridotomy is a treatment for narrow-angle glaucoma. In laser iridotomy, a small hole is placed in the iris to create a hole for fluid to drain from the back of the eye to the front of the eye. Without this new channel through the iris, intra-ocular pressure can build rapidly causing damage to the delicate optic nerve, and permanent loss of vision. In most patients, the iridotomy is placed in the upper portion of the iris, under the upper eyelid, where it cannot be seen.

A small hole is placed in the iris to create a hole for fluid to drain from the back of the eye to the front of the eye.
The purpose of an iridotomy is to preserve vision, not to improve it.
Laser iridotomy is for those:
Realistic expectations:
Serious complications with laser iridotomy are extremely rare, but like any medical procedure, it does have some risks. The chance of losing vision following a laser procedure is extremely small. The main risks of a laser iridotomy are that your iris might be difficult to penetrate, requiring more than one treatment session. Another risk is that the hole in your iris will close. This happens in less than one-third of the cases.
Following your procedure, you may still require medications or other treatments to keep your eye pressure sufficiently low. This additional treatment will be necessary if there was damage to the trabecular meshwork prior to the iridotomy or if you also have another type of glaucoma in addition to the closed-angle type.
If you and your doctor decide that laser iridotomy is an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
If you would like more information about this procedure you can make an appointment or contact the office for additional information.
 The outer layer of the eye can be divided into three areas: the cornea, the sclera, and the limbus. The cornea is the clear part, or the window, that covers the iris and the pupil. The sclera is the white part of the eye. The limbus is the thin area that connects the cornea and the sclera.
The outer layer of the eye can be divided into three areas: the cornea, the sclera, and the limbus. The cornea is the clear part, or the window, that covers the iris and the pupil. The sclera is the white part of the eye. The limbus is the thin area that connects the cornea and the sclera.
Limbal relaxing incisions (LRIs) treat low to moderate degrees of astigmatism. As the name suggests, the surgeon makes small relaxing incisions in the limbus, which allows the cornea to become more rounded when it heals. LRIs are placed at the very edge of the cornea (in the limbus) on the steepest meridians. LRIs are often combined with other surgical and laser vision correction procedures and cataract surgery.
Limbal Relaxing Incisions are for those:
Realistic expectations:
The decision to have LRIs is an important one that only you can make. The goal of any refractive surgical procedure is to reduce your dependence on corrective lenses. However, we cannot guarantee you will have the results you desire.
Serious complications to LRIs are extremely rare. If you decide that LRIs are an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
Alternatives to LRIs
LRIs are not the only surgical procedure designed to correct astigmatism. To learn about other procedures go to the vision correction procedures section of our Web Site. If you would like to learn more about vision correction procedures from sources other than our practice, we encourage you to link to a number of Web sites we feel provide factual and up-to-date information. You may also choose to make an appointment, attend a seminar or request additional information to learn more.
See “Vision Correction” above.
See “Vision Correction” above.
A posterior capsulotomy is a non-invasive laser procedure to eliminate the cloudiness that occasionally interferes with a patient’s vision after cataract surgery. In modern cataract surgery, the cataract is removed, but a thin membrane that held the cataract is left in place to hold the implanted artificial lens.Leaving the capsule in place during cataract surgery is a great advancement because it allows the vision after surgery to be more stable and ensures fewer surgical complications. However, sometimes the posterior or back portion of the capsule becomes cloudy over time. This can be resolved with a quick in-office laser procedure.

The capsular bag can become cloudy over time.
A posterior capsulotomy is for those who:
Realistic expectations:
Serious complications with posterior capsulotomy are extremely rare. It is a safe and effective procedure, but like any medical procedure, it does have some risks. Going to an eye specialist experienced with the procedure can significantly minimize the risks involved with posterior capsulotomy.
If you and your doctor decide that posterior capsulotomy is an option for you, you will be given additional information that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
If you would like more information about this procedure you can make an appointment or contact the office for additional information.
See “Vision Correction” above.
One way to alleviate dry eye is to help the eyes to make better and longer use of the small amount of lubricating tears they do produce. This is accomplished by closing off the small funnel-like drain hole found in the inner corner of the upper and lower eyelids. These drain holes, called punctums, can be closed with tiny plugs called punctal plugs. The plugs can be placed in the two tear ducts, top, and bottom, in both eyes or in only the lower ducts. The punctum can also be permanently closed with a heat or laser procedure.

Punctal plugs can be temporary or permanent. Temporary plugs dissolve a few days after insertion. If your dry eye symptoms disappear when the temporary plugs are inserted, your doctor may consider permanent punctal occlusion.
Punctal occlusion is for those:
Realistic expectations:
Serious complications with punctal occlusion are extremely rare, but like any medical procedure, it does have some risks. If you experience side effects, your doctor can remove the plugs. Going to a specialist experienced in punctal occlusion can significantly minimize risks.
If you and your doctor decide that punctal occlusion is an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed.
If you would like more information about this procedure you can make an appointment or contact the office for additional information.
See “Vision Correction” above.
Laser surgery has become increasingly popular as an intermediate step between medications and traditional glaucoma filtration surgery. Selective Laser Trabeculoplasty (SLT) is a relatively new laser treatment for open-angle glaucoma. SLT uses short pulses of low energy laser light to target melanin-containing cells in a network of tiny channels, called the trabecular meshwork. The objective of the surgery is to help fluids drain out of the eye, reducing intraocular pressure that can cause damage to the optic nerve and loss of vision.
The selective technique is much less traumatic to the eye than Argon Laser Trabeculoplasty (ALT), which has been the standard laser procedure. ALT can cause tissue destruction and scarring of healthy cells in the trabecular meshwork structure. SLT reduces intra-ocular pressure without this risk. SLT can be used to effectively treat some patients who could not benefit from ALT. This includes patients who have already been treated with ALT.
Although your doctor may suggest laser surgery at any time, it is often performed after trying to control intra-ocular pressure with medicines. In many cases, you will need to keep taking glaucoma drugs even after laser surgery.
SLT is for those:
Realistic expectations:
The effect of the surgery may wear off over time. Serious complications with SLT are extremely rare, but like any surgical procedure, it does have some risks. Going to a specialist experienced in SLT can minimize the risks.
If you and your doctor decide that SLT is an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction. If you would like more information about this procedure you can make an appointment or contact the office for additional information.

Astigmatism, unlike normal vision, occurs when the cornea is shaped like a football (more curved in one direction than the other) and often occurs in combination with myopia (nearsightedness) and hyperopia (farsightedness). This causes light to focus in more than one point on the retina, resulting in blurry and distorted vision.
Symptoms of astigmatism:
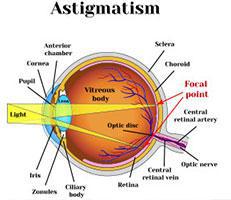
Causes of astigmatism:
Diagnosing astigmatism:
Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Treatment of astigmatism:
Glasses and contact lenses are used by many for the temporary treatment of astigmatism. However, there are a number of vision correction procedures that can surgically reduce or eliminate astigmatism.
Other types of refractive errors include nearsightedness, farsightedness, and presbyopia.
 Blepharitis means inflammation of the eyelids. Some doctors call it granulated eyelids. Almost everyone gets blepharitis at some time in his or her life. Some people get it repeatedly. Fortunately, blepharitis is relatively easy to treat.
Blepharitis means inflammation of the eyelids. Some doctors call it granulated eyelids. Almost everyone gets blepharitis at some time in his or her life. Some people get it repeatedly. Fortunately, blepharitis is relatively easy to treat.
Types of blepharitis:
Staphylococcus blepharitis is caused by a germ called Staphylococci, commonly known as “staph.” It often begins in childhood and continues throughout adulthood. This form of the condition results in collar scales on lashes, crusting, and chronic redness at the lid margin. Dilated blood vessels, loss of lashes, sties, and chalazia (nodules on the eyelids) also occur.
Seborrhea blepharitis is the most common and least severe form of this condition. It is not an infection but is caused by improper function of the oil glands, which causes greasy, waxy scales to accumulate along the eyelid margins. Seborrhea may be a part of an overall skin disorder that affects other areas. Hormones, nutrition, general physical condition, and stress are factors in seborrhea.
Ulcerative blepharitis is a less common but more severe condition that may be characterized by matted, hard crusts around the eyelashes, which, when removed, leave small sores that may bleed or ooze. There may also be a loss of eyelashes, distortion of the front edges of the eyelid,s and chronic tearing.
In severe cases, the cornea, the transparent covering of the front of the eyeball, may also become inflamed.
Symptoms of blepharitis:
Causes of blepharitis:
Treating blepharitis:
In addition to eliminating redness and soreness, treatment can prevent potential infection and scarring of the cornea. You doctor will perform a complete eye examination to determine the most effective treatment.
Cleaning
Usually, blepharitis can be controlled by careful, daily cleaning of the eyelashes. You can do this by moistening a clean washcloth with tap water as warm as you can stand without burning. Hold the washcloth against the eyelids until it cools, then rewarm and repeat for five to ten minutes.
After soaking, scrub each eyelid gently for one minute using a clean washcloth wrapped around your index finger and moistened with warm tap water. Cotton-tipped applicators, like Q-tips, are also useful to remove accumulated material from the eyelashes.
To remove excessive amounts of material from your eyelids, use a few drops of a non-irritating shampoo, such as baby shampoo, mixed in lukewarm water. Being careful to avoid getting shampoo in your eye, scrub back and forth along the eyelashes of all eyelids, and then rinse with plain tap water. Once the redness and soreness are under control, this cleaning may be decreased from daily to twice weekly. However, if the symptoms return, return to daily cleansing immediately.
Medication
In some cases, your doctor may prescribe eye drops or ointment to be used along with the daily cleansing regimen. For ointments, use a clean fingertip to rub a small amount into the eyelashes. Be careful to follow recommended dosages; excess medication will cause temporary blurring of vision. And with any medication, there is a small possibility of allergy or other reaction. If you think this is happening, stop the medication and contact your doctor immediately.
For certain types of blepharitis, medications taken by mouth are helpful. Most of these medications are antibiotics that also improve or alter the oil composition of the eyelid oil glands. When taken properly, they are safe. However, side effects may occur in some individuals, including skin rash, slight nausea, and increased sensitivity to the sun.
Although medications may help control the symptoms of blepharitis, they alone are not sufficient; keeping the eyelids clean is essential.
If you think you may have blepharitis, your eye doctor can determine the cause and recommend the right combination of treatment specifically for you.
See “Senior Eye Health” above.
The cornea is the clear, outer window of the eye. A corneal abrasion is simply a scratch in the epithelium (skin), or the thin, outer layer of the cornea. Abrasions usually heal in a short time period, sometimes within hours. Deeper or larger scratches may take up to a week. The cornea has a tremendous number of nerve endings, which makes any damage to the cornea very painful.

A corneal abrasion is simply a scratch in
the outer layer of the cornea
Symptoms of corneal abrasions:
Causes of corneal abrasions:
Diagnosing corneal abrasions:
Your eye doctor can identify corneal abrasions by examining your eyes with magnifying instruments. Your doctor will check your eye, including under your eyelid, to make sure there is no foreign material present. Depending on the initial exam, fluorescein dye may be used to help locate and identify the corneal abrasions. A test called the Seidel test (painting the wound with dye and observing for leakage) may be performed to uncover possible deeper injuries.
Treating corneal abrasions:
Your doctor may apply a topical anesthesia to help relieve the pain. Usually, a tight patch will be placed over the eye and if the abrasion is small, the epithelium should heal overnight. If the abrasion is large, it may take a few days and your doctor may prescribe antibiotics to help prevent infections. It is important that you do not rub your eye, especially during the healing process.
 The cornea is the clear front window of the eye. It transmits light to the interior of the eye allowing us to see clearly. Corneal disease is a serious condition that can cause clouding, distortion and eventually blindness. There are many types of corneal disease. The three major types are keratoconus, Fuchs’ endothelial dystrophy, and bullous keratopathy.
The cornea is the clear front window of the eye. It transmits light to the interior of the eye allowing us to see clearly. Corneal disease is a serious condition that can cause clouding, distortion and eventually blindness. There are many types of corneal disease. The three major types are keratoconus, Fuchs’ endothelial dystrophy, and bullous keratopathy.
Symptoms of corneal disease:
Keratoconus is a weakening and thinning of the central cornea. The cornea develops a cone-shaped deformity. Progression can be rapid, gradual or intermittent. Keratoconus usually occurs in both eyes, but can occur in only one eye.
Fuchs’ endothelial dystrophy is a hereditary abnormality of the inner cell layer of the cornea called the endothelium. The purpose of this layer is to pump fluids out of the cornea, keeping it thin and crystal clear. When the endothelium is not healthy, fluids are not pumped out and the cornea develops swelling, causing it to become cloudy and decrease vision.
Bullous keratopathy is a condition in which the cornea becomes permanently swollen. This occurs because the inner layer of the cornea, the endothelium, has been damaged and is no longer pumping fluids out of the tissue.
Causes of corneal disease:
Diagnosing corneal disease:
Your eye doctor can check for corneal disease and trauma by examining your eyes with magnifying instruments. Using a slit lamp and advanced diagnostic technology such as corneal topography, your doctor can detect early cataracts, corneal scars, and other problems associated with the front structures of the eye. After dilating your eyes, your doctor will also examine your retina for early signs of disease.
Treatment for corneal disease:
As with any serious eye infection, corneal disease should be treated immediately. Although corneal transplant is almost always the necessary treatment to restore vision when the cornea becomes clouded, there are other measures that can be taken to prolong vision in the early stages of the disease.
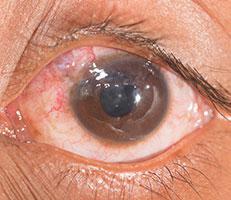 The front portion of the eye is covered with a thin, transparent membrane called the cornea, which protects the interior of the eye. If there is a break or defect in the surface layer of the cornea, called the epithelium, and damage to the underlying stroma, a corneal ulcer results. The ulcer is usually caused by microorganisms, which gain access to the stroma through the break in the epithelium.
The front portion of the eye is covered with a thin, transparent membrane called the cornea, which protects the interior of the eye. If there is a break or defect in the surface layer of the cornea, called the epithelium, and damage to the underlying stroma, a corneal ulcer results. The ulcer is usually caused by microorganisms, which gain access to the stroma through the break in the epithelium.
Corneal ulcers generally heal well if treated early and aggressively. However if neglected, corneal clouding and even perforation (a hole in the cornea) may develop, resulting in serious loss of vision and possibly loss of the eye. Corneal ulcers are a serious vision-threatening condition and require prompt medical attention.
Symptoms of corneal ulcers:
Causes of corneal ulcers:
Diagnosing corneal ulcers:
Corneal ulcers are a serious vision-threatening condition and require prompt medical attention. If left unattended, corneal ulcers may penetrate the cornea, allowing infection to enter the eyeball, which can cause permanent loss of vision and possible loss of the eye. Your eye doctor can identify corneal ulcers by examining your eyes with magnifying instruments and performing a culture study to identify infection. Your doctor will check your eye, including under your eyelid, to make sure there are no foreign materials present. Depending on the initial exam, fluorescein dye may be used to identify the corneal defects. A test called the Seidel test (painting the wound with dye and observing for leakage) may be performed to uncover possible deeper injuries.
Treatment for corneal ulcers:
If treated early, corneal ulcers are usually curable in two to three weeks. They are typically treated with antibiotic eye drops. Sometimes, topical steroids will also be used to decrease the risk of scarring and inflammation.
Diabetes is a disease that affects blood vessels throughout the body, particularly vessels in the kidneys and eyes. When the blood vessels in the eyes are affected, this is called diabetic retinopathy.
The retina is in the back of the eye. It detects visual images and transmits them to the brain. Major blood vessels lie on the front portion of the retina. When these blood vessels are damaged due to diabetes, they may leak fluid or blood and grow scar tissue. This leakage affects the ability of the retina to detect and transmit images.
During the early stages of diabetic retinopathy, reading vision is typically not affected. However, when retinopathy becomes advanced, new blood vessels grow in the retina. These new vessels are the body’s attempt to overcome and replace the vessels that have been damaged by diabetes. However, these new vessels are not normal. They may bleed and cause the vision to become hazy, occasionally resulting in a complete loss of vision. The growth of abnormal blood vessels on the iris of the eye can lead to glaucoma. Diabetic retinopathy can also cause your body to form cataracts.
The new vessels also may damage the retina by forming scar tissue and pulling the retina away from its proper location. This is called retinal detachment and can lead to blindness if left untreated.
Symptoms of diabetic retinopathy:
Causes of diabetic retinopathy:
You can reduce your risk of developing diabetic retinopathy by:
Diagnosing diabetic retinopathy:
There are usually no symptoms in the early stages of diabetic retinopathy. Vision may not change until the disease becomes severe. An exam is often the only way to diagnose changes in the vessels of your eyes. This is why regular examinations for people with diabetes are extremely important.
You eye doctor may perform a test called fluorescein angiography. During the test, a harmless orange-red dye called Fluorescein will be injected into a vein in your arm. The dye will travel through your body to the blood vessels in your retina. Your doctor will use a special camera with a green filter to flash a blue light into your eye and take multiple photographs. The pictures will be analyzed to identify any damage to the lining of the retina or atypical new blood vessels.
Treatment for diabetic retinopathy:
Diabetic retinopathy does not usually impair sight until the development of long-term complications, including proliferative retinopathy (when abnormal new blood vessels bleed into the eye). When this advanced stage of retinopathy occurs, pan-retinal photocoagulation is performed. During this procedure, a laser is used to destroy all of the dead areas of retina where blood vessels have been closed. When these areas are treated with the laser, the retina stops manufacturing new blood vessels, and those that are already present tend to decrease or disappear.
If diabetic retinopathy has caused your body to form cataracts, they can be corrected with cataract surgery.
See “Senior Eye Health” above.
The name “dry eye” can be a little confusing since one of the most common symptoms is excessive watering! It makes more sense, though, when you learn that the eye makes two different types of tears.
 The first type, called lubricating tears, is produced slowly and steadily throughout the day. Lubricating tears contain a precise balance of mucous, water, oil, nutrient proteins, and antibodies that nourish and protect the front surface of the eye.
The first type, called lubricating tears, is produced slowly and steadily throughout the day. Lubricating tears contain a precise balance of mucous, water, oil, nutrient proteins, and antibodies that nourish and protect the front surface of the eye.
The second type of tear, called a reflex tear, does not have much lubricating value. Reflex tears serve as a kind of emergency response to flood the eye when it is suddenly irritated or injured. Reflex tears might occur when you get something in your eye, when you’re cutting onions, when you’re around smoke, or when you accidentally scratch your eye. The reflex tears gush out in such large quantities that the tear drainage system can’t handle them all and they spill out onto your cheek. Still another cause of reflex tearing is irritation of the eye from lack of lubricating tears. If your eye is not producing enough lubricating tears, you have dry eye.
Symptoms of dry eye:
Causes of dry eye:
Diagnosing dry eye:
Your eye doctor can check for dry eye by examining your eyes with magnifying instruments, measuring your rate of tear production and checking the amount of time it takes for tears to evaporate between blinks. The doctor can also check for pinpoint scratches on the front surface of the eye caused by dryness using special, colored eyedrops call fluorescein or Rose Bengal.
Treatments for dry eye:
The most common treatment is the use of artificial teardrops that help make up for the lack of natural lubricating tears. Artificial tear products come in liquid form, longer lasting gel form, and long-lasting ointment form, which is most often recommended for nighttime use. Many different brands of artificial tears are available over-the-counter. Some contain preservatives and some do not. Unpreserved tears may be recommended for people whose eyes are sensitive to preservatives. Artificial tears can generally be used as often as needed, from a few times per day to every few minutes. You should follow the regimen your doctor recommends.
When infection, inflammation of the eyelids or clogged oil glands contribute to dry eye, special lid cleaning techniques or antibiotics may be recommended. It may also help to avoid hot, dry or windy environments or to humidify the air in your home or office.
Restasis and Xiidra are topical medications for Dry Eye Disease. Both drops help the eyes produce more tears by reducing inflammation, which is often a cause of dry eye.
Punctal occlusion is a medical treatment for dry eye that may enable your eyes to make better and longer use of the few lubricating tears they do produce.
TrueTear is a novel medical device that delivers gentle neurostimulation to the lacrimal nerve in the nose to generate more tears.
See “Senior Eye Health” above.
 Hyperopia, unlike normal vision, occurs when the cornea is too flat in relation to the length of the eye. This causes light to focus at a point beyond the retina, resulting in blurry close vision and occasionally blurry distance vision as well. Usually, this condition is undetected until later in life because the young eye is able to compensate for the hyperopia by contracting the internal lens of the eye.
Hyperopia, unlike normal vision, occurs when the cornea is too flat in relation to the length of the eye. This causes light to focus at a point beyond the retina, resulting in blurry close vision and occasionally blurry distance vision as well. Usually, this condition is undetected until later in life because the young eye is able to compensate for the hyperopia by contracting the internal lens of the eye.
Symptoms of hyperopia:
Causes of hyperopia:
Diagnosing hyperopia:
Many people are not diagnosed with hyperopia without a complete eye exam. School screenings typically do not detect this condition because they test only for distance vision. Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Treatment of hyperopia:
Glasses and contact lenses are used by many for the temporary treatment of hyperopia. However, there are a number of vision correction procedures that can surgically reduce or eliminate hyperopia.
Other types of refractive errors include nearsightedness and presbyopia.
Flashes and floaters can be alarming. Usually, however, an eye examination will confirm that they are harmless and do not require any treatment.
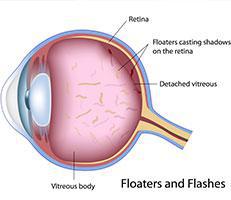
Flashes & Floaters
Symptoms of flashes & vitreous floaters:
Causes of flashes and floaters:
Aging of the eye: Most flashes and floaters are caused by age-related changes in the gel-like material, called vitreous, that fills the back of the eye.
When you are born, the vitreous is firmly attached to the retina. In the very young, the vitreous is rather thick, like firm gelatin. Within the vitreous, there may be clumps of gel or tiny strands of tissue debris left over from the eye’s early development. These clumps or strands are firmly embedded in the thick, young vitreous and cannot move around much.
As you get older, the vitreous gradually becomes thinner or more watery. By the time you are in your twenties or thirties, the vitreous may be watery enough to allow some of the clumps and strands to move around inside the eye. This material floating inside the eye can cast shadows on the retina, which you see as small floating spots.
Sometime after about age 55, you may experience the onset of larger, more bothersome floaters or flashes of light. By this age, the vitreous gel has usually become much more watery. It jiggles around quite a bit when you move your eye, making flashes and floaters much more common.
Eventually, the aging vitreous can pull away from the retina and shrink into a dense mass of gel in the middle of the eyeball. Shadows cast onto the retina by the detached vitreous can cause you to see large floaters.
Who is at risk?
Flashes and floaters are very common. Almost everyone experiences them at one time or another. They become more frequent as we age. In rare cases, a doctor’s exam may reveal a more serious problem called a retinal tear or retinal hole, so it’s important to get regular eye exams and inform your doctor if you’re experiencing flashes or floaters.
Diagnosing flashes and floaters:
Using special instruments to look into your eyes, your doctor can distinguish between harmless floaters and flashes and more serious retinal problems such as holes, tears or detachment. The usual symptoms of these more serious problems include seeing hundreds of small floating spots, persistent flashing lights, or a veil-like blockage of a portion of the vision. If you experience any of these, you should contact your doctor immediately.
Treatment for flashes and floaters:
There is no way to eliminate the floater through surgery, laser treatment or medication. With time, the floater will become less noticeable as the brain adjusts to its presence and can “tune out” the floater. The floater will always be somewhat observable and present, particularly if one eye is covered and the patient looks at a light-colored background.
Anyone with flashes or the sudden onset of a new floater should be examined promptly by an ophthalmologist. The ophthalmologist will perform a dilated exam and look at the vitreous and retina with specialized equipment. Sudden flashes or floaters could be symptoms of a vitreous detachment, which is a benign condition that carries the risk of developing into a retinal tear and/or retinal detachment.
Overview
The cornea is the clear “window” in the front of the eye that allows light rays to enter.
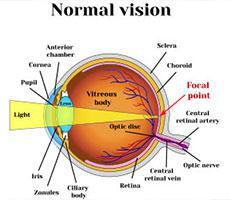
If the endothelium does not function normally, then water moves into the cornea causing swelling. Swelling causes clouding of the cornea and blurred vision. The more corneal swelling or “edema,” the more severely the vision is blurred. Eventually, the outer corneal layer (epithelium) also takes on water, resulting in pain and more severe vision impairment. Epithelial swelling reduces vision by changing the normal curvature of the cornea. It causes a sight-limiting haze to develop. Epithelial swelling may also form small “blisters” on the corneal surface. When these “blisters” burst, extreme pain can occur.The cornea has three layers – the outer epithelium (or skin), a middle area called stroma and a delicate, single-celled inner lining called the endothelium. The endothelium acts as a barrier to prevent water inside the eyeball from moving into and swelling the other layers of the cornea. The cells of the endothelium actively pump water from the cornea back into the eye.
Once lost, endothelial cells do not grow back. The remaining cells spread out to cover the empty spaces, trying to pump water from a larger area. The pump system becomes less efficient, causing corneal clouding, swelling and eventually, reduced vision. Fortunately, most people have enough endothelial cells throughout life to prevent corneal swelling or edema.
Fuchs’ Dystrophy
Fuchs’ dystrophy (named after Dr. Fuchs) is an inherited condition that affects the delicate inner layer (endothelium) of the cornea. Patients with Fuchs’ dystrophy have endothelial cells that:
Fuchs’ dystrophy affects both eyes and is slightly more common in women than men. On average, half of the family members of an affected person may carry or suffer from the condition. The exact cause of Fuchs’ dystrophy is unknown. Hereditary, hormonal and inflammatory factors probably all play a role.
Signs and Symptoms
In early stages, people with Fuchs’ dystrophy may wake up with blurred vision, which gradually clears over the day. That’s because during the day, water continuously evaporates from the surface of the eye and is replaced with water drawn from the inner compartments of the eye. Overnight, when we sleep with closed eyes, water cannot evaporate from the surface of the eye and accumulates in the cornea, causing slight swelling which blurs vision. Once eyes are opened throughout the day, evaporation reduces the water content and the thickness of the cornea, allowing for clearing of vision. In later stages, as the dystrophy worsens, evaporation is not enough to remove accumulated water in the cornea, and swelling and blurred vision last all day.
Typical complaints among people with Fuchs’ dystrophy include:
Treatment
Fuchs’ dystrophy cannot be cured. Doctors are unable to treat the endothelial cells to make them work better or to become more numerous. However, blurred vision resulting from the corneal swelling can be controlled with medication. Salt solutions containing sodium chloride (Muro 128 drops or ointment, 2% or 5%) are often prescribed to draw fluid from the cornea and reduce swelling. Steroid eye drops may be helpful in specific situations.
Another simple technique that reduces moisture in the cornea is to hold a hair dryer at arm’s length, blowing air towards the face with the eyes open. This warm airflow increases evaporation of water from the cornea, temporarily decreases swelling, and may improve vision. Often very helpful in early stages, this technique may not be effective when swelling is severe, as in advanced stages.
Fuchs’ Dystrophy in Patients with Cataracts
As people age, the lens within the eye often becomes cloudy, developing into a cataract. Cataract surgery is very common and has a very high success rate. Any eye surgery causes some damage to the delicate endothelial cell layer of the cornea, causing a reduction in the number of cells remaining to pump water from the cornea. If the number of endothelial cells is insufficient following cataract surgery, corneal swelling will develop, reducing vision. Corneal transplantation may be necessary to recover vision. When patients with Fuchs’ dystrophy develop cataracts, it is important to carefully evaluate the status of the endothelium to decide whether the cornea is likely to continue to function well following cataract surgery. A recommendation may be made to combine cataract surgery with corneal transplantation. One combined surgery can achieve what would otherwise require two separate surgeries with a longer post-operative recovery.
More details about this combined surgery are available from your surgeon.
Corneal transplantation is considered when vision deteriorates to the point that it interferes with daily activities and impairs a person’s ability to function normally. This surgery replaces the full thickness of the cornea, including the endothelium, with healthy layers. The cloudy cornea is replaced with clear corneal tissue.
Keratoconus, often referred to as “KC” is an eye disease that causes the cornea to become progressively thinner. A normal cornea is round or spherical in shape, but with keratoconus the cornea bulges forward, assuming more of a cone shape. As light enters the cone-shaped cornea it is bent and distorted and unable to come to a point of clear focus on the light-sensitive retina.
Keratoconus usually affects both eyes but the two eyes often progress at different rates. This disease typically begins during teenage years. In most patients, it progresses for several years before stabilizing in the third to fourth decade of life. In severe cases, it can continue to worsen. In these cases, the cornea continues to thin and bulge outward, further blurring vision. Scarring of the cornea can also develop.
Symptoms of keratoconus:
Who is at risk:
Researchers believe that approximately three million people worldwide have keratoconus. It affects males and females of all races throughout the world. The causes are still being researched, but the likelihood of developing keratoconus is greater if you:
Treatment
In mild cases, glasses and soft contacts can be effective, but in more advanced cases, these no longer work well.
Gas permeable (GP) contact lenses
These are the primary treatment for keratoconus. To counteract the distortion of the cornea, most keratoconus patients require special GP lenses to provide a smooth surface that can focus light in place of their own cornea’s distorted surface. Because the pattern of distortion in keratoconus is as unique as a fingerprint, the GP lenses are custom prescribed and manufactured.
A proper contact lens fitting is crucial to ensure optimal vision, comfort, and eye health. Poor fitting lenses can lead to corneal abrasions, scarring, and infection.
Corneal Crosslinking
This procedure strengthens the cornea to reduce the progression of keratoconus. The treatment consists of applying riboflavin to the cornea and then exposing the cornea to a special ultraviolet light source, which creates strong bonds within the corneal tissue.
Surgery
Many keratoconus patients will never require surgery, but it is an option in severe and advanced cases. If your doctor determines you have significant scarring of the cornea, he or she may recommend corneal transplant surgery. In this procedure, the scarred tissue is replaced with a section of donated cornea that is clear. About 10 to 20% of keratoconus patients will eventually require a corneal transplant. However, corneal transplantation is not a cure. Following a successful corneal transplant, most patients still need glasses, soft contacts, or GP lenses for adequate vision.
Intacs prescription inserts
Your doctor may recommend a relatively new surgery for keratoconus using Intacs prescription inserts. This surgery is sometimes called intrastromal corneal ring segment implantation. It is a procedure for patients who can’t wear GP lenses but whose disease has not progressed to the point of needing to have a corneal transplant. During this surgery, tiny plastic segments are placed inside the cornea beneath the surface to reduce nearsightedness and astigmatism. Normally, eyeglasses are still required after the procedure to give you the best possible vision.
Precautions
Patients with keratoconus must not have LASIK or PRK laser eye surgery due to an unacceptable risk of a poor outcome. The cornea in keratoconus is unusually thin and weak. For patients with keratoconus, LASIK surgery thins and weakens their corneas further. This can irreversibly destabilize the cornea and accelerate its distortion. Rubbing the eyes may also increase the progression of keratoconus. Eye rubbing can often be very vigorous with patients using excessive force with their knuckles. Corneas already weakened by inflammation may develop thinning and protrusion as a result of rubbing.
For More Information
Your eye doctor is the best resource for specific questions about your diagnosis and treatment. Remember that regular eye examinations are crucial for preserving your eye health and vision. For general information, visit Center for Keratoconus at www.keratoconus.com.
See “Senior Eye Health” above.
During childhood, people with normal vision have the ability to focus on objects as close as their nose and also on objects very far away. They can rapidly, without conscious thought, switch focus from near to far vision. This is called accommodation. As each year passes, that ability to focus and to switch focus decreases. By the time most people reach their forties, they need an aid, such as reading glasses or bifocals, to focus on objects close up. This condition is called presbyopia.
Monovision is a technique where one eye (usually the dominant eye) is corrected for clear distance vision, and the other eye is corrected for comfortable near vision. Monovision allows a person to see close objects clearly with one eye and distance objects clearly with the other eye. The vision part of the brain tends to filter out the image from the eye that is not in clear focus, so those who have monovision eventually do not pay attention to the eye that is not as clearly focused. Those who have monovision are often able to see well enough both at distance and near to do things at any age without corrective lenses.
Monovision can be achieved with contact lenses or with vision correction procedures by correcting the non-dominant eye for near vision and the dominant eye for distance vision. If you are considering a vision correction procedure, your doctor can put you into monovision contact lenses so you can try it before you permanently correct your eyes with monovision.
Most people’s brains automatically get used to monovision within a couple of weeks or months. In our experience, most people over the age of 40 to 45 who try monovision and take the time to fully become accustomed to it, like it and find it very useful.
See “Senior Eye Health” above.
 Myopia, unlike normal vision, occurs when the cornea is too curved or the eye is too long. This causes light to focus in front of the retina, resulting in blurry distance vision.
Myopia, unlike normal vision, occurs when the cornea is too curved or the eye is too long. This causes light to focus in front of the retina, resulting in blurry distance vision.
Myopia is a very common condition that affects nearly 30 percent of the U.S. population. It normally starts to appear between the ages of eight and 12 years old, and almost always before the age of 20. As the body grows, the condition often worsens. It typically stabilizes in adulthood.
Symptoms of myopia:
Causes of myopia:
Diagnosing myopia:
Many times, myopia is diagnosed during school screenings. Sometimes parents notice that their children are having difficulty seeing street signs or the television. Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Treatment of myopia:
Glasses and contact lenses are used by many for the temporary treatment of myopia. However, there are a number of vision correction procedures that can surgically reduce or eliminate myopia.
Other types of refractive errors include nearsightedness, farsightedness, and presbyopia.
The human eye gives us the sense of sight, allowing us to learn more about the surrounding world than any of the other five senses. The eye allows us to see and interpret the shapes, colors and dimensions of objects by processing the light they reflect or give off.
The cornea (the clear window on the front of the eye) and the lens of the eye (the transparent structure inside the eye) are both critical to normal vision. The goal of these two lenses is to focus light onto a layer on the back of the eye known as the retina. As light enters into the eye it is focused by the cornea and the lens so that images appear clearly on the retina. The retina then transmits these images to the brain where they are processed.
If the images focus perfectly on the retina, this results in 20/20 vision; focusing in front or behind the retina results in nearsightedness or farsightedness. If the cornea is shaped like a football instead of a sphere, this is called astigmatism. When any of these conditions occurs, images are perceived by the brain as being blurry. This is due to “refractive error,” which means the eyeball is not the right size or the cornea does not have the right curve. Presbyopia is a vision condition in which the lens loses its flexibility, making it difficult to focus on close objects.
See “Senior Eye Health” above.
 Conjunctivitis is an inflammation of the conjunctiva, the thin, transparent membrane covering the surface of the inner eyelid and the front of the eye. The conjunctiva has many small blood vessels. It lubricates and protects the eye while the eye moves in its socket. When the conjunctiva becomes inflamed, this is called conjunctivitis.
Conjunctivitis is an inflammation of the conjunctiva, the thin, transparent membrane covering the surface of the inner eyelid and the front of the eye. The conjunctiva has many small blood vessels. It lubricates and protects the eye while the eye moves in its socket. When the conjunctiva becomes inflamed, this is called conjunctivitis.
Bacterial conjunctivitis, often called pink eye, typically causes swelling of the eyelid and a yellowish discharge. Sometimes it causes itching and/or matting of the eyelids. Bacterial conjunctivitis is very contagious and can be easily transmitted by rubbing the eye and then infecting household items such as towels or handkerchiefs. It is common for entire families to become infected.
Symptoms of conjunctivitis:
How can conjunctivitis be prevented?
Certain precautions can to taken to avoid the disease and stop its spread. Careful washing of the hands, the use of clean handkerchiefs, and avoiding contagious individuals are all helpful. Children frequently get conjunctivitis because of their poor hygiene.
If you or someone in your household has contracted conjunctivitis, follow these steps to prevent the spread of the infection:
Diagnosing conjunctivitis:
Your eye doctor can easily detect conjunctivitis at an exam.
Treatment for conjunctivitis:
Antibiotic drops and compresses can ease discomfort and clear up the infection, normally within just a few days. Sometimes, the inflammation does not respond well to the initial treatment with eye drops. In those rare cases, a second visit to the office should be made. When there is a severe infection, oral antibiotics are necessary. If left untreated, conjunctivitis can create serious complications such as infections in the cornea, eyelids and tear ducts.
Presbyopia is a vision condition in which the lens loses its flexibility, making it difficult to focus on close objects. During the early and middle years of life, the crystalline lens of the eye has the ability to focus both near and distant images by getting thicker for near objects and thinner for distant objects. When this ability is lost, presbyopia results.
Symptoms of presbyopia:
Causes of presbyopia:
Age: As we age, the lenses in the eyes lose some of their elasticity, and without elasticity, they lose some of their ability to change focus for different distances. Presbyopia may seem to occur suddenly, but the actual loss of flexibility takes place over a number of years. Long before an individual is aware that seeing close up is becoming more difficult, the lenses in the eyes have begun losing their ability to flatten and thicken. Only when the loss of elasticity impairs vision to a noticeable degree is the change recognized. Presbyopia usually becomes noticeable in the early to mid-forties.
Diagnosing presbyopia:
A comprehensive examination will include testing for presbyopia. Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Treatment of presbyopia:
Reading glasses and contact lenses are used by many for the temporary treatment of presbyopia. However, there are a number of vision correction procedures that can surgically reduce or eliminate the effects of presbyopia. Some presbyopic patients like monovision, which allows them to see distance clearly in one eye and close-up clearly with the other eye.
Presbyopia can be present in combination with other types of refractive errors such as nearsightedness, farsightedness, and astigmatism.
A pterygium is a fleshy triangular tissue that grows over the cornea, usually on the inner corner of the eye. Sometimes, it grows big enough that it interferes with vision. As the pterygium develops, it may alter the shape of the cornea, causing astigmatism.
Symptoms of a pterygium:
Causes of a pterygium:
The exact cause of pterygia isn’t known, but it’s thought to be linked to:
Diagnosing a pterygium:
Chances are, you’ll notice a pterygium. Your eye doctor can also diagnose it during a routine eye exam.
Treatment of a pterygium:
Eye drops or ointment can be used to reduce the irritation caused by a pterygium. If the pterygium grows over the central cornea, impairing site, it can be removed surgically. Prevention is important. It’s a good idea to protect your eyes with sunglasses if you’ll be in the sun or a dusty, dry environment.
Retinal detachment occurs when the retina is lifted or pulled from the wall of the eye. If not treated immediately, a retinal detachment can cause permanent vision loss. A retinal detachment is a medical emergency. Anyone experiencing the symptoms of a retinal detachment should call the office immediately.
Symptoms of retinal detachment
Who is most at risk for retinal detachment?
Treatment for retinal detachment
Retinal detachments are treated with surgery that may require a hospital stay. In some cases, a scleral buckle, a tiny synthetic band, is attached to the outside of the eyeball to gently push the wall of the eye against the detached retina. If necessary, a vitrectomy may also be performed. Vitrectomy is a procedure in which the vitreous humor is removed and replaced with a gas that pushes the retina back onto the wall of the eye. Over time the eye produces fluid that replaces the gas. In both of these procedures, either a laser or a cryopexy (a freezing device) is used to “weld” the retina back in place.
There are veins in the retina that drain blood out of the retina, back to the heart. If those veins become blocked, this can cause fluid leakage, which can lead to vision loss. If you experience a sudden loss of your central vision or a blurry or missing area of vision, call our office at once.
Symptoms of retinal vein occlusion
Causes of retinal vein occlusion
Treatment for retinal vein occlusion
The type of treatment depends on the cause of the blockage and the extent of damage. A laser can be used to reduce leakage and the growth of abnormal new blood vessels.
Strabismus is a condition in which the eyes point in different directions. Types of strabismus include crossed eyes (esotropia), out-turned eyes (exotropia), or vertical misalignment (hyper or hypotropia). The turning of the eye may be constant or may show up only some of the time. Strabismus should be evaluated and treated.
Symptoms of strabismus
Causes of strabismus
Strabismus is caused by a lack of coordination between the eyes. In children, the cause of strabismus is not known, although the condition runs in families and occurs more commonly in children with neurological problems.
In adults, causes of strabismus include injury to an eye muscle or the nerves controlling those muscles; head trauma; conditions such as diabetes or high blood pressure; loss of vision; an eye or brain tumor; Graves’ disease, stroke or other muscle and nerve disorders.
Treating Strabismus
Children with strabismus must be identified and treated at a young age in order to prevent permanent vision problems. In children, when the two eyes fail to focus on the same image, the brain may learn to ignore the input from one eye. If this is allowed to continue, the eye that the brain ignores will never see well. Children do not grow out of strabismus.
Treatment options depend upon the type of strabismus and may include glasses, patching one eye, prism lenses, and/or surgery.
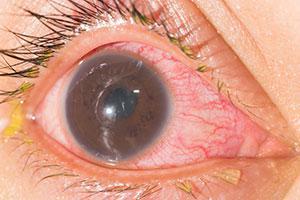 Uveitis is an inflammation that affects a part of the eye called the uvea. The uvea provides most of the blood supply to the retina. Uveitis causes spotty areas of scarring that can lead to vision loss. The degree of vision loss depends on the amount and location of the scarring.
Uveitis is an inflammation that affects a part of the eye called the uvea. The uvea provides most of the blood supply to the retina. Uveitis causes spotty areas of scarring that can lead to vision loss. The degree of vision loss depends on the amount and location of the scarring.
Symptoms
Causes
Many conditions, diseases, and infections can lead to the development of uveitis. In some cases, the cause is unknown. Uveitis usually affects people between 20-50 years of age.
Diagnosing Uveitis
Uveitis is diagnosed with a thorough internal examination of the eye. Near and distance vision, plus intraocular pressure are also evaluated. In some cases, blood tests are performed to check for underlying disease or infection.
Treating uveitis
The appropriate treatment for uveitis is determined by the severity of the disease and which eye structures are involved. Uveitis is typically treated with topical eye drops and/or oral medications to reduce inflammation. Sometimes, medication is required to lower the intraocular pressure, too. If complications are advanced, surgery may be necessary.
After the inflammation has gone down, such as scar tissue, cataracts, and glaucoma that have resulted from uveitis may need to be treated.

Botox injection is a revolutionary wrinkle reduction procedure that can reduce or eliminate wrinkles in the upper third of the face, including forehead lines, frown lines between the eyes, and crow’s feet around the eyes. It is not surgery. There is no chance of scarring.
Botox is a protein that weakens and inactivates muscles that wrinkle the skin. When Botox is injected in extremely small doses directly into a specific muscle, it blocks the signals from the brain from reaching the muscle. As the muscle weakens, the skin overlying the muscle relaxes and the wrinkles caused by muscle contractions soften and often disappear. The effect can last from 4 to 5 months.
Botox injection is for those who:
Before Your Treatment:
Ask your doctor to determine if you are a candidate for Botox injection. Together, you will determine the number and regularity of treatments best for you.
Realistic Expectations:
Botox, when used in these extremely small doses, has a high level of safety. Since Botox proteins are only attracted to muscles, it has no effect on the central nervous system. It does not cause numbness in the area of the injections, and muscles related to other facial expressions are rarely affected. One or two patients in every hundred may experience a temporary drooping of the eyelid, but this usually goes away in a week or two.
Serious complications with Botox injection are extremely rare, but like any medical procedure, it does have some risks. Going to a specialist experienced in Botox injection can significantly minimize the risks. The vast majority of our patients are extremely happy with their appearance after Botox injection, however, we cannot guarantee you will have the results you desire.
If you decide that Botox injection is an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
Alternatives to Botox Injection:
Chemical peels and cosmetic surgery have been the primary means of reducing the undesirable effects of aging and wrinkles. To learn about other cosmetic procedures, please visit the cosmetic procedures section of our Web Site.
Botox is a registered trademark of Allergan, Inc.
Latisse™ is the first and only FDA-approved prescription eyelash growth treatment proven to grow your own natural eyelashes longer, fuller, and darker…is now available at our office.
Latisse Menlo Park and Palo Alto California
For more information about Latisse, visit their website (www.latisse.com).
See “Senior Eye Health” above.
See “Senior Eye Health” above.
